The Skeletal System
Chemical Composition (Living Part)
1. Organic Components:
a) Osteoid- 35% of bone- soft material made of protecoglycan & collagen fibers
*Allows bone to bend/gives flexibility (resists tension/bending forces)
b) Bone Cells:
i) Osteoblasts- create/build bone by making osteoid
ii) Osteoclasts-(similar to macrophages) break down by releasing acid enzymes (work with Osteoblasts to rebuild bone).
2. Inorganic Components:
Hydroxyapatites---65% of bone->3 types calcium, mainly Ca Phosphate.
***Significance: Harden Osteoid-> responsible for hardness of bone; Helps bone resist compression (crushing forces).
Organic Components
a) Osteoid- 35% of bone- soft material made of protecoglycan & collagen fibers
* Allows bone to bend/gives flexibility (resists tension/bending forces)
b) Bone Cells--
i) Osteoblasts- create/build bone by making osteoid,
ii)Osteocytes- lose ability to make bone
iii) Osteoclasts-(similar to macrophages) uses acids & enzymes to break down bone during repair & rebuilding(remodeling)
Osteoid
35% of extracellular matrix-soft material made of proteoglycan & collagen fibers
*Allows bone to bend/gives flexibility (resists tension/bending forces)
Bone Cells
*Osteoblasts- create/build bone by making osteoid, once surrounded by bone they have made, becomes osteocytes.
*Osteocytes-lose ability to make bone, maintain existing bones, uses "arms"-DENDRITIC EXTENSTIONS to send nutrients to each other.
*Osteoclasts-(similar to macrophage) uses acid & enzymes to break down bone during repair & rebuilding(remodeling).*Work with Osteoblasts to rebuild bone).
Inorganic Components (Non-Living)
Hydroxyapatites (mineral salts)---65% of extracellular matrix->3 types of calcium, mainly Ca Phosphate.
***Significance:Hardens bone tissue, Osteoid-> responsible for hardness of bone; Helps bone resist compression (crushing forces).
Organization of bone matrix
1. The matrix is organized into layers of bone called lamellae <-(layers)
a.) In compact bone(designed to with stand stress from one direction), there are three types of lamellae:
*Osteons (concentric lamellae)
*Interstitial Lamellae-(incomplete layers) fragments/pieces of old osteons formed during remodeling.
*Circumferntial Lamellae- bony layer that underlies the perisotem or endosteum.
b.) In cancellous/spongy bone, the lamellae form trabeculae, or narrow branches that connect together to form a loose web or net structure. *Can bear stress from multiple different directions
organization of bone matrix con...
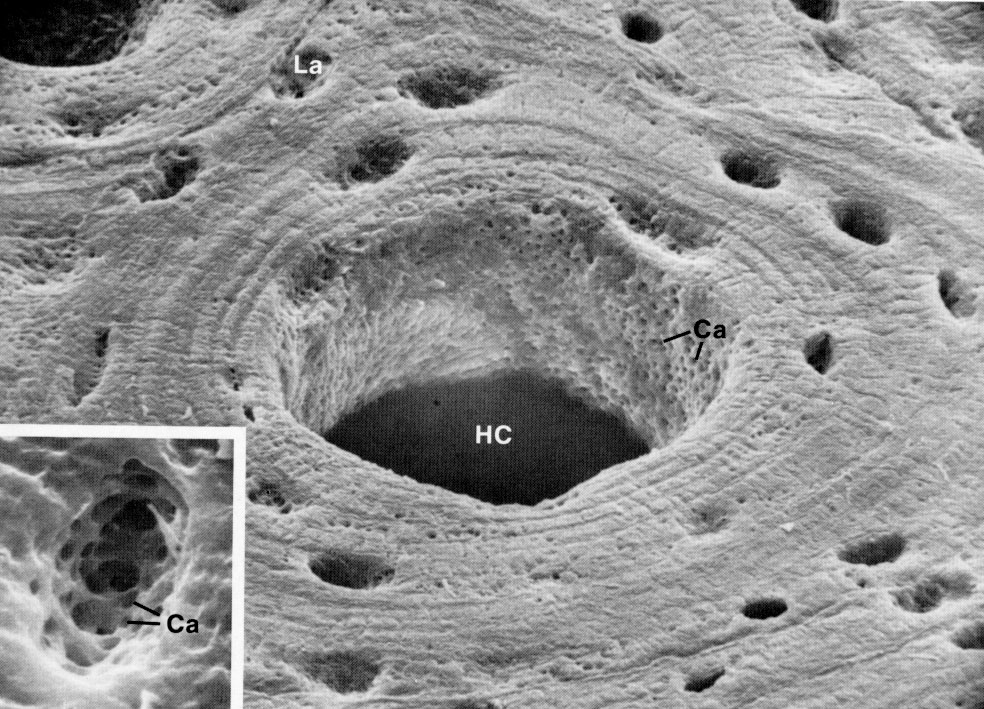
2. Within the matrix of both (compact and cancellous bone) osteocytes are found in holes called Lacunae. The dendritic extensions<-(branching) of each osteocyte are found in tiny crack-like passageways called canaliculi.
3. Blood vessels and nerves are found in Haversian/Central Canals, located in the center of osteons (parallel to bone shaft), and in Perforating/Volkmann's Canals (perpendicular or transverse to bone shaft).
Bone Anatomy
A. Diaphysis
B. Epiphysis
C. Metaphysis/Growth Plate
D. Articulation
E. Medullary Cavity (Bone Marrow Cavity)
F. Periosteum
Diaphysis
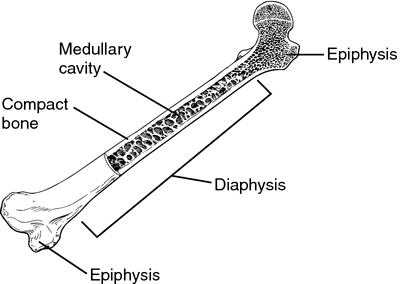
The hollow shaft made of compact bone
Epiphysis

The round ends, filled with spongy bone and covered by outer layer of compact bone
Metaphysis/Growth Plate

Band of hyaline cartilage, area located between diaphysis and epiphysis. Before puberty contains the epiphyseal growth plate. After puberty, when the growth plate disappears, contains the epiphyseal line (scar where growth plate was).
*allows for growth in bone length
Articulation
Where two or more bones come together to form a joint
Medullary Cavity (Bone Marrow Cavity)
1. Red Bone Marrow/Myeloid Tissue-(Reticular C.T.) The birthplace of RBC's and WBC's; Located throughout skeleton of children but only in select locations of adult skeleton.
Major-Pelvic bone, Top epiphyes of femor, humerous.
Miner locations; Vertabrae, ribs, skull
2. Yellow Bone Marrow- Primarily adipose (fat) tissue; Most myeloid tissue turns into this.
3. Endosteum (inside)--Membrane made of a single layer of osteoblasts and osteoclasts which lines the medullary cavity and covers trabeculae of spongy bone' Essential because it provides bone cells needed for growth, remodeling, and repair of bone.
Periosteum(around)
Covers outer surface of bones
1. Outer Layer--Dense irregular collagenous tissue; important because tendons (& therefore muscle) attach to this tissue. Sharpey's fibers (perforating fibers) attach the periosteum to tendons and ligaments, forming strong connections to them.
2. Inner layer--Single layer of osteoblast; Essential because it provides bone cells needed for bone growth, remodeling, and repair.
Formation of Bone in the Early Skeleton
Overview
The skeleton of a human embryo is made of two tissues that will gradually be turned into bone. The process of making bone is called ossification.-->formation of bone
Intramembranous ossification
*Forms bone from a soft membrane (tissue) made of collagen (similar to dense/fiborus tissue) called MESENCHYME, (embryonic tissue)
*Forms flat bones of skull, & Clavicles
*Process complete by age 2
Endochondral ossification
*Forms bones from hyaline cartilage;(Hyaline remains in growth plates after birth)--> allow skeleton to grow in length.
*Forms rest of skeleton
*Process complete by end of puberty
Intramembranous ossification Steps
All of the flat skull bones and the clavicles are made from a fiborous connective tissue called mesenchyme.
STEP 1: Ossification centers (REGIONS OF BONE FORMATION) appear in the mesenchyme.(area where bones beginning to be made-osteoblast)
a.) Osteoblast cells produce the bone matrix, or osteoid.
*b.) Spongy bone, or woven bone, grows and expands as a series of trabeculae that grow outward freom the ossification centers.
c.) Blood vessels grow into the woven bone as it forms.
Intramembranous ossification Steps con...
STEP 2: The periosteum forms on the surface of the bone.
*provides the osteoblast on the surface so the next step can happen.
STEP 3: Compact bone(AkA Bony Collar->surface layer) forms beneath the periosteum.
STEP 4: Blood vessels inside the bone turn into Red bone marrow.
***The skull bones are not fully ossified (turned into bone) at birth. They become ossified around age 2. Until then, the parts of these bones which are still mesenchyme are called FONTANELS or "soft spots"
Endochondral ossification IN THE FETUS
All other bones are formed from an entirely different tissue--hyaline cartilage.
STEP 1: cartilage occurs by TWO METHODS:
a. Appositional Growth--cartilage cells on surface of the existing cartilage multiply and produce matrix. causing growth of the cartilage on its surface.
b. Interstitial Growth--Cartilage cells in the center of the existiong cartilage multiply and produce matrix, causing growth of the cartilage from within.(in btwn)
STEP 2: The periosteum forms on the surface of the cartilage.
STEP 3: Compact bone forms beneath the periosteum.
STEP 4: Calcification and cavitation occur in the center of the cartilage.
Hypertrophy of the chondrocytes occurs before this step begins. the cartilage cells enlarge before they add calcium carbonate to the cartilage. causing their own death and therefore creating holes (cavities) in the cartilage. Adding calcium to the cartilage kills it so that it can be replaced with bone.
Endochondral ossification IN THE FETUS con...
STEP 5: Primary Ossicfication Centers appear.
a.The periosteal bud invades the cavities and spongy bone forms. The bud, a blood vessel, grows into the hole in the center of the cartilage, bringing along with it osteoblasts that will start primary ossification centers. These centers will produce spongy bone in the diaphysis (shaft)
b. The diaphysis elongates, thinkens, and a medullary cavity forms.
STEP 6: Secondary Ossification Centers appear.Shortly before or after birth, these centers develop and turn the cartilage of the epiphyses into spongy bone. At birth, hyaline cartilage remains at only two locations.
1.) Growth plates-metaphyses
2.) On the surface of the epiphyses, called articular cartilage.
Bone Types
1. Bone is organized into layers called lamellae.
a) In compact bone, the lamellae form circular patterns: Osteons (Concentric lamellae) -->Target pattern-> made of circular rings.
*Designed to with stand stress from one direction
b) In cancellour/spongy bone, the lamellae from trabeculae, or narrow branches that connect together to form a loose web or net structure.
2. Blood vessels and nerves are found in Haversian Canals, located in the center of osteons, and in Perforating/Volkmann's Canals which lie at right angles to the Haversian Canals. in same direction as bone shaft. (parallel)
Compact Bone

There are three types of lamellae:
*Osteons (concentric lamellae)- Target patterns-> made of circular rings
*Interstitial Lamellae-(incomplete layers)-> fragments/pieces of old osteons formed during remodeling.
*Circumferntial Lamellae- bony layer that underlies the perisotem or endosteum.
--Designed to with stand stress from one direction
Cancellous/spongy bone
The lamellae form trabeculae, or narrow branches that connect together to form a loose web or net structure. *Can bear stress from multiple different directions
BONE GROWTH IN LENGTH in the GROWTH PLATES
The long bones of the skeleton can grow in length up until 18-21 years of age because endochondral ossification occurs within the growth plates during that time.
The steps in the formation of bone can be seen in the CELL LAYERS OF THE GROWTH PLATES (METAPHYSES):
1) Zone of Resting or Reserve Cartilage (nearest to epiphysis)
2) Zone of Proliferation-Cartilage growth
3) Zone of Hypertrophy
4) Zone of Calcification
Bone Growth in DIAMETER
Besides growing in length, bones must also grow in diameter in the young adult. Growth in diameter is accomplished by growth of the actual bone, NOT by growth of the cartilage in the growth plate (metaphysis).
Bone has appositional growth but NOT interstitial grwoth
*1.) Can't expand from within b/c it is calcified (harden).
*2.) Bone can only be added to surfaces (inside & outside) b/c osteoblasts are...not found in shaft, only on outer surface (periosteum) & inner surface (endosteum).
Bone REMODELING
IN GENERAL:
The simultaneous break down (reabsorption) by osteoclast & rebuilding (depostion) by osteoclast.These processes should occur @ equal rates. (or u'll end up with osteoporosis)
*1/5 of skeleton is remodeled every yr. Epiphyses (ends) of femur are most frequently rebuilt, is dependent upon levels of activity' creates interstitial lamellae.
PURPOSES for Remodeling
A. To adjust bone to stress- is slight bending of bone caused by skeletal muscle contraction.Causes tiny electrical charges (currents) that "tell" the bone cells how to remodel.
B. To increase Length and Diameter of Medullary Cavity as bone grows
PURPOSES for Remodeling con...
C. To Regulate Calcium levels in the body
Ca is crucial for:
*proper electricity in nerves & brain
*proper organ functions
*proper skeletal & Cardiac muscle construction
*proper blood clothing
Calcium Homeostasis (How bone regulates Ca levels)
(Keeping Calcium @ steady level)
A. Roles of Osteoblasts and Osteoclasts
1. Osteoblasts create new bone and in the process cause calcium to deposited in the bone because it leaves the bloodstream and enters the forming bone. Thus, they reduce/lower calcium levels in the blood.
2. Osteoclasts break down bone and in the process cause calcium to be released from the bone. Thus, they increase/raise calcium levels in the blood.
Influence of Hormones
1. Parathyroid Hormone (PTH)--Its job is to prevent hypocalcemia (too LITTLE calcium)
*Most important of the 2 hormones b/c low Ca is deadly-> it causes skeletal muscle spasms & paralysis-> death by asphyxiation.
PTH raises calcium levels in THREE ways:
a. Effect on the Intestines
b. Effect on Kidneys
c. Effect on Bone
Influence of Hormones
PTH raises calcium levels in THREE ways:
Effect on the INTESTINES
--> Getting Ca from food
1) This effect is PTH's way of increasing the body's natural process that brings Ca into the body/blood. PTH increases the absorption of calcium by the intestines.
2) This action is reinforced by one of PTH's effects on the kidneys.
Influence of Hormones
PTH raises calcium levels in THREE ways:
Effect on the KIDNEYS
->lose with kidneys by uren
1) The first effect is PTH's way of decreasing any natural process that causes Ca loss in body: PTH decreases urinary loss of calcium by the kidneys, called calcium excretion.
2) The second effect on the kidneys helps the INTESTINES absorb calcium; PTH increases Vitamin D produciton by the kidneys. Without enough Vitamin D, the intestines can't bring calcium into the body-it's an essential part of the process.
Influence of Hormones
PTH raises calcium levels in THREE ways:
Effect on BONE
1) This effect is PTH's way of releasing stored Ca (in bones) in the body that has a surplus of it: PTH causes the bones to release calcium.
2) To do this, PTH increases osteoclasts activity (bone breakdown) because the only way bones can release their extra store of calcium is to dissolve them.
Only 1% Ca in bone is available for release-called exchangeable Ca
Influence of Hormones
Calcitonin Hormone
It's job is to prevent hypercalcemia (too MUCH calcium)--> more rare, rarely leads to death
strange hormone b/c it's not very good at it's job.
*Calcitonin levels are high only in children, (for growth of skeleton) except during pregnancy--> levels rise to protect mom's bones.
Lowers Calcium levels in TWO ways:
Major action: Decrease Osteoclast activity
Weak secondary action: Increase osteoblast activity
Influence of Hormones
Calcitonin Hormone-
Lowers Calcium levels in TWO ways:Major action
*Major action: Decrease(slows down) Osteoclast activity (bone breakdown) to stop the release of calcium from bones. (If calcium levels are high, there doesn't need to be extra calcium coming out of the bones).
Influence of Hormones
Calcitonin Hormone-
Lowers Calcium levels in TWO ways:Weak secondary action
Weak secondary action: Increase osteoblast activity (bone building). As new bone is made, calcium is pulled into the bones to harden them, which lowers calcium levels in the blood.
*used as treatment for osteoporosis- but still not highly effective
Articulations and their Movements
A. Major Types Of Movement:
1. Flexion & Extension
2. Abduction & Adduction
3. Supination & Pronation
B. Articulations
1. Fibrous Joints
2. Cartilagenous Joints
3. Synovial Joints
FIBROUS JOINTS
1.) General Description
a. Small (usually) ligaments join the two bones
b. No movement--synarthrotic-->(together Joint)
2.) Sutures--Seams between skull bones(which are attached via tiny ligaments)
3.) Syndesmoses---Joint in the gap between radius & ulna, tibia & fibula
4.) Gomphoses---Joint between the teeth and teeth sockets-Nail shape
CARTILAGENOUS JOINTS
1.) Synchondroses---Hyaline Cartilage-(btwn bones)-Synarthrotic No movement
a.) Epiphyseal Growth Plates
b.) First Sternocostal Joint--1st rib's connection(via costal cartilage) to sternum
Synostoses-joint where 2 or more bones fuse into one bone/piece EX: Growth plates/Sutures
CARTILAGENOUS JOINTS con...
2.) Symphyses---Fibrocartilage *amphiarthrothic-"btwn joint" limited movement
a. Intervertebral Discs-pads btwn
b. Symphysis Pubis
c. Sternal Angle
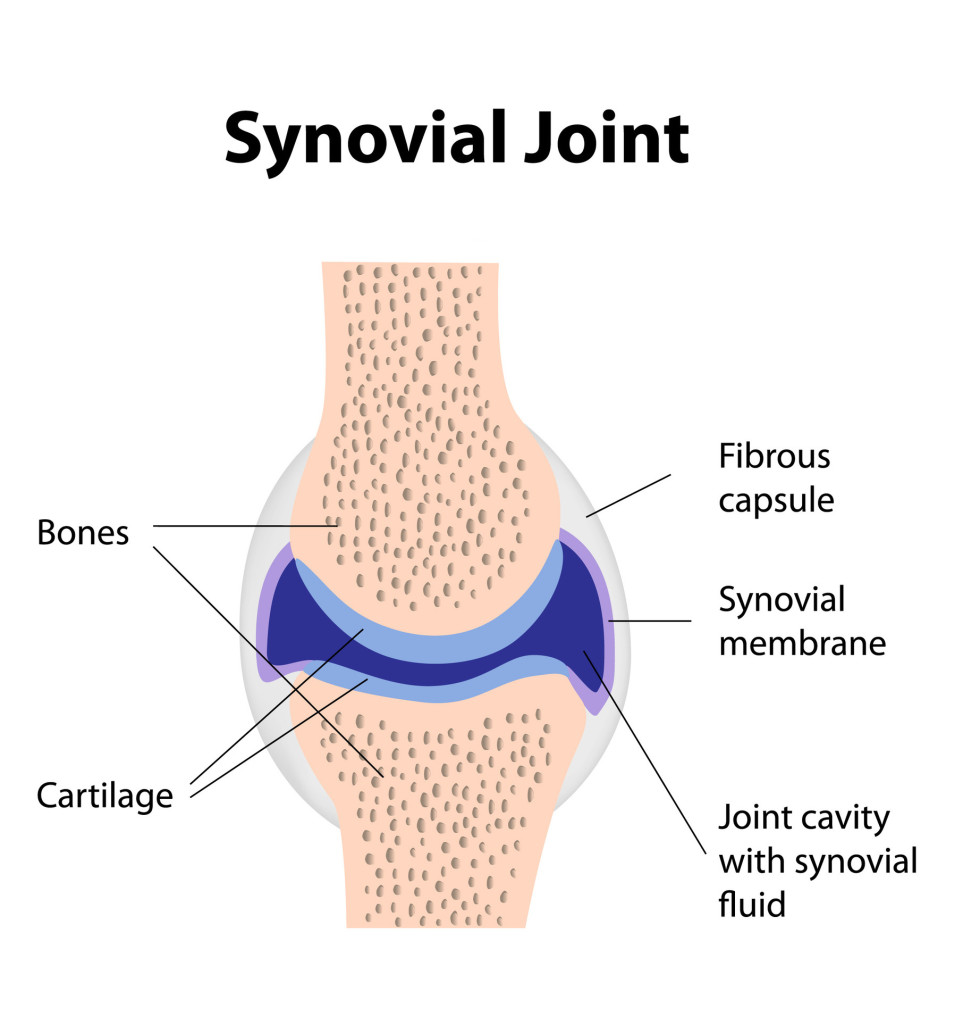
*SYNOVIAL JOINTS
*Has cartilage(articular) hyaline also but it moves
General Description
a. Allows for Free Movement-diarthrotic
b. Contain a Joint Cavity-A space between the bones, created by a joint capsule(inner layer) and filled with synovial fluid(synovial membrane)
c. Contain Large Ligaments
d. Contain Bursae-"Sacks" of fluid-filled synovial membrane located where tendons and ligaments rub against bone-> Protects tendons & ligaments
e. Contain Articular Cartilage--Hyaline cartilage on epiphyseal bone surfaces where bones make contact/rub together
f. May Contain Menisci--Disc of fibrocartilage that floats between the bones of the knee joint
Major types of Movements
A. Flextion & Extension
B. Abduction & Adduction
C. Supination & Pronation

Flexion, Extension & Hyperextension

Flexion= To bend a limb; also an anterior movement-Forwards
Extention= To straighten a limb; Also a movement that returns the body part to the anatomical position; Also a posterior movement-backwards
Hyperextesion= Movement behind/posterior to anatomical position.
Ex: looking up, bending backwards at waist.Moving arm or leg behind the body.
FLEXION
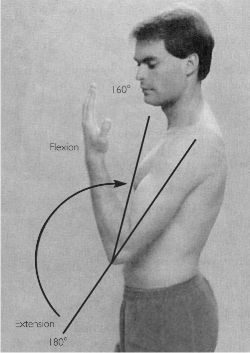
To bend a limb; also an anterior movement-Forwards
EXTENSION

To straighten a limb; Also a movement that returns the body part to the anatomical position; Also a posterior movement-backwards
HYPEREXTENSION

Movement behind/posterior to anatomical position.
Ex: looking up, bending backwards at waist.Moving arm or leg behind the body.
Abduction & Adduction
Abduction= To move a part laterally, away from the midline of the body-OUTWARD
Adduction= To move a part medially, toward the midline of the body-INWARD
ABDUCTION

To move a part laterally, away from the midline of the body-OUTWARD
ADDUCTION

To move a part medially, toward the midline of the body-INWARD
*Supination & Pronation
Supination= To rotate the forearm so that the palm faces upward
Pronation= To rotate the forearm so that the palm faces downward
SUPINATION

To rotate the forearm so that the palm faces upward
PRONATION

To rotate the forearm so that the palm faces downward

*Synovial Joints
1. General description:
a. Allows for Free Movement-->diarthrotic
b. Contain a Joint Cavity---A space between the bones, created by a joint capsule (Inner layer) and filled with synovial fluid,(synovial membrane).
c. Contain large ligaments
d. Contain Bursa---A "Sacks" of fluid-filled synovial membrane located where tendons and ligaments rub against bone (cushioning)-proteccts tendons & ligaments from damage(rubbing).
e. Contain Articular Cartilage--Hyaline cartilage on epiphyseal bone surfaces where bones can make contact/rub together
f. May Contain Menisci--Disc of fibrocartilage that floats btwn the bones of the knee joint

Types of Synovial Joints
a. Plane/Gliding Joint---Two flat articulating bone surfaces
> Nonaxial Movement: Small slipping or gliding movements only-least movement of all synovial types.
*1) Intercarpal Joints (between wrist bones)
2) Sternoclavicular joint (btwn sternum & clavicle)
*3) Intervertebral joints (btwn articular processes of vertebrae)
4)Sacroiliac Joint (btwn sacrum and iliac bones)
b. Hinge Joint---Rounded process of one bone fits into concave surface of other bone-Door movements (front 2 back)
>Uniaxial Movement:-> Movement in one plane (axis)-allows flexion & extention (front 2 back) only
1) Knee joint
*2) Elbow Joint-(btwn Humerous & ulna)
3) Interphalangeal joints (btwn finger & toe bones)
Types of Synovial Joints, Cont...1
c.Pivot Joint(half-rotation)--- One bone has a round process that is held by a ring ligament to the 2nd bone; allowing first bone to rotates
>Uniaxial Movement:Rotation back & forth in one plane (axis)
1) Atlanoaxial joint(2nd neck joint; btwn atlas & axis, first two cervical vertebrae)
2)Elbow joint (btwn head of radius & ulna--allows for rotation of the forearm)
*Both uniaxial types are in elbow.
d. Saddle Joint---One bone surface is concave(curves towards back) while the other is convex (curves forward)
Biaxial Movement: Movement in two planes-Front 2 Back (flexion & extension) & side 2 side (abduction & adduction)
**Thumb Joint: (1st carpometacarpal joint)
Types of Synovial Joints, Cont...2
e. Ball & Socket---Round bone process fits into indention of second bone
> Triaxial/Multiaxial Movement:Movement in three planes, one of which is rotation (has most movement of all synovial types).
**Shoulder and hip joints
f. Ellipsoid/Condyloid(oval shaped)---Modified ball and socket where "ball" is oval rather than round
> Biaxial Movement: Movement in two planes
1) Atlanto-occipital joint (1st neck joint btwn occipital condyles and atlas)
2) Knuckles (btwn metacarpals and phalanges)
3) Btwn radius & carpals at wrist
Type of Synovial Joint: Plane/Gliding

Two flat articulating bone surfaces
> Nonaxial Movement: Small slipping or gliding movements only-least movement of all synovial types.
*1) Intercarpal Joints (between wrist bones)
2) Sternoclavicular joint (btwn sternum & clavicle)
*3) Intervertebral joints (btwn articular processes of vertebrae)
4)Sacroiliac Joint (btwn sacrum and iliac bones)
Type of Synovial Joint: Hinge Joint

Rounded process of one bone fits into concave surface of other bone-Door movements (front 2 back)
>Uniaxial Movement:-> Movement in one plane (axis)-allows flexion & extention (front 2 back) only
1) Knee joint
*2) Elbow Joint-(btwn Humerous & ulna)
3) Interphalangeal joints (btwn finger & toe bones)
Type of Synovial Joint: Pivot Joint

One bone has a round process that is held by a ring ligament to the 2nd bone; allowing first bone to rotates
>Uniaxial Movement:Rotation back & forth in one plane (axis)
1) Atlanoaxial joint(2nd neck joint; btwn atlas & axis, first two cervical vertebrae)
2)Elbow joint (btwn head of radius & ulna--allows for rotation of the forearm)
*Both uniaxial types are in elbow.

Type of Synovial Joint: Saddle Joint
One bone surface is concave(curves towards back) while the other is convex (curves forward)
>Biaxial Movement: Movement in two planes-Front 2 Back (flexion & extension) & side 2 side (abduction & adduction)
**Thumb Joint: (1st carpometacarpal joint)

Type of Synovial Joint:Ball & Socket

Round bone process fits into indention of second bone
> Triaxial/Multiaxial Movement:Movement in three planes, one of which is rotation (has most movement of all synovial types).
**Shoulder and hip joints
Type of Synovial Joint:Ellipsoid/Condyloid

(oval shaped)---Modified ball and socket where "ball" is oval rather than round
> Biaxial Movement: Movement in two planes
1) Atlanto-occipital joint (1st neck joint btwn occipital condyles and atlas)
2) Knuckles (btwn metacarpals and phalanges)
3) Btwn radius & carpals at wrist
Osteons(Concentric lamellae)
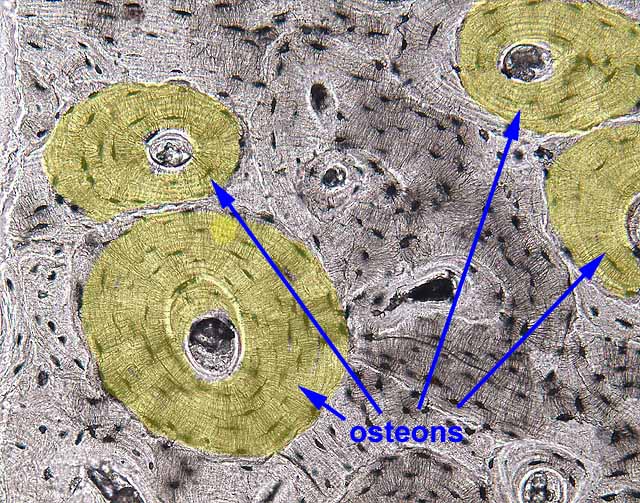
Target pattern-> made of circular rings
*Designed to withstand stress form one direction
Interstitial Lamellae

(Incomplete layers)-Fragments/pieces of old osteons formed during remodeling.
Circumferential Lamellae
bony layer that underlies the periostem or endosteum.
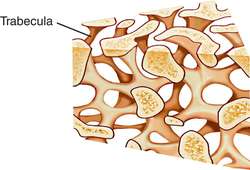
Cancellous/spongy bone

The lamellae form trabeculae or narrow branches that connect together to form a loose web or net structure.
*Can bear stress from multiple different directions
Haversian Canals
Blood vessels & nerves are found here, Located in the center of osteons (parallel to bone shaft), & in Perforating/ Volkmann's Canals (perpendicular or transverse to bone shaft)
Lacunae

Holes within the matrix of both (compact & cancellous bone) where osteocytes are found.
Canaliculi
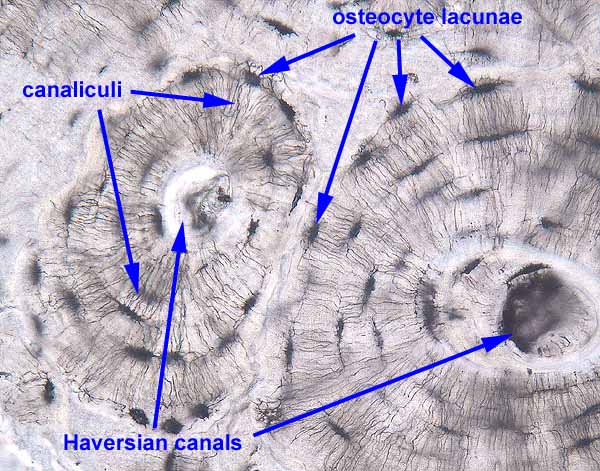
Tiny crack-like passageways where the dendritic extentions of each osteocyte are found.
Bone Anatomy

Diaphysis Bone

The hollow shaft made of compact bone
Epiphysis Bone
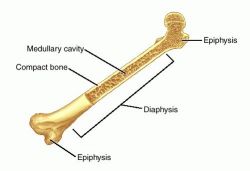
Rounded ends,filled with spongy bone and covered by outer layer of compact bone
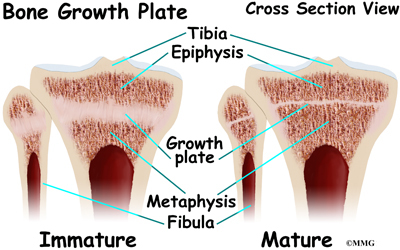
Metaphysis/Growth Plate
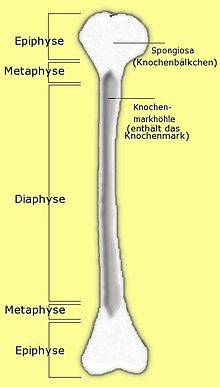
Band of hyaline cartilage, area located between diaphysis and epiphysis. Before puberty contains the epiphyseal growth plate. After puberty, when the growth plate disappears, contains the epiphyseal line (scar where growth plate was).
*allows for growth in bone length
Articulation

Where two or more bones come together to form a joint.
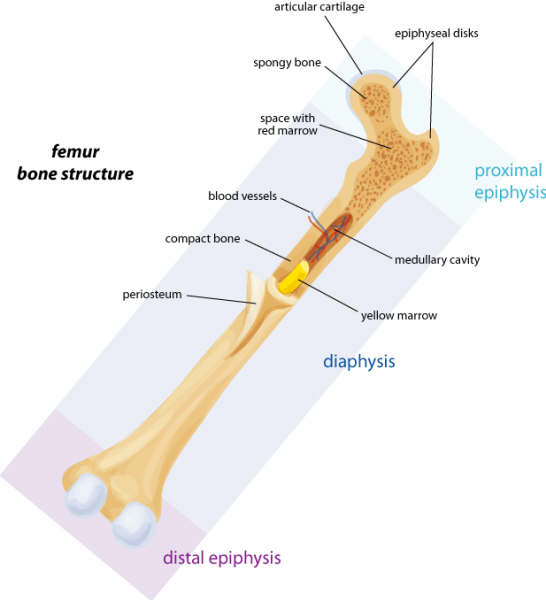
Medullary Cavity

(Bone Marrow Cavity)
1. Red Bone Marrow/Myeloid Tisssue(reticular C.T.)- the birthplace of RBC's and WBC's; Located throughout skeleton of children but only in select locations of adult skeleton.
Location in adults; Major:pelvic bone, top epiphyes of humerus,femur; Minor locations; vertabrae, ribs, skull
2. Yellow Bone Marrow Primarily fat tissue; Most myeloid tissue turns into this.
Fibrous Joint: Sutures
Seams between skull bones (which are attached via tiny ligaments)
Fibrous Joint: Syndesmosis

Joints between tibia & fibula and between radius & ulna
Flexion

To bend a limb; also an anterior movement
Extension
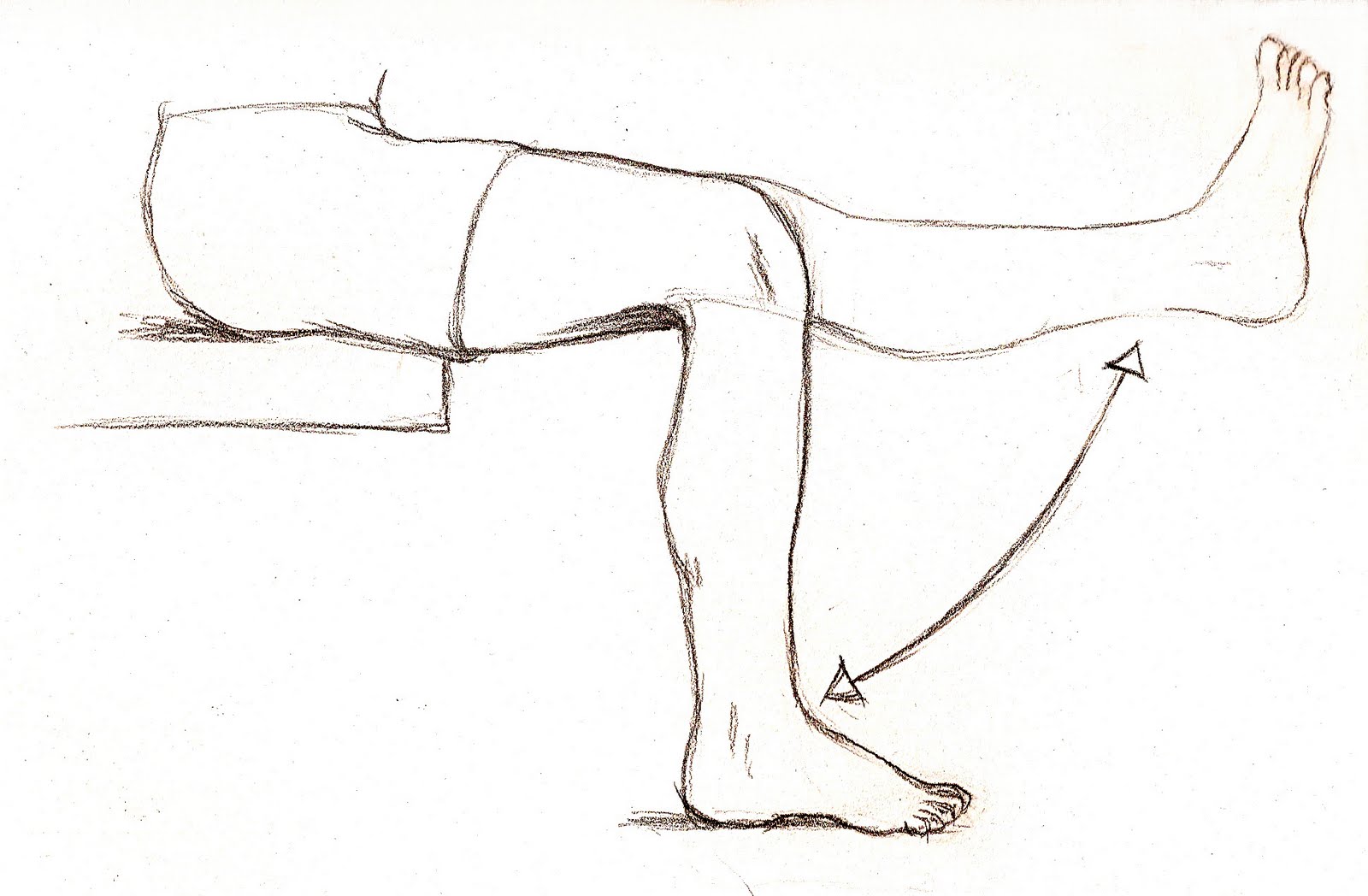
To straighten a limb; Also a movement that returns the body part to the anatomical position; Also a posterior movement
Abduction
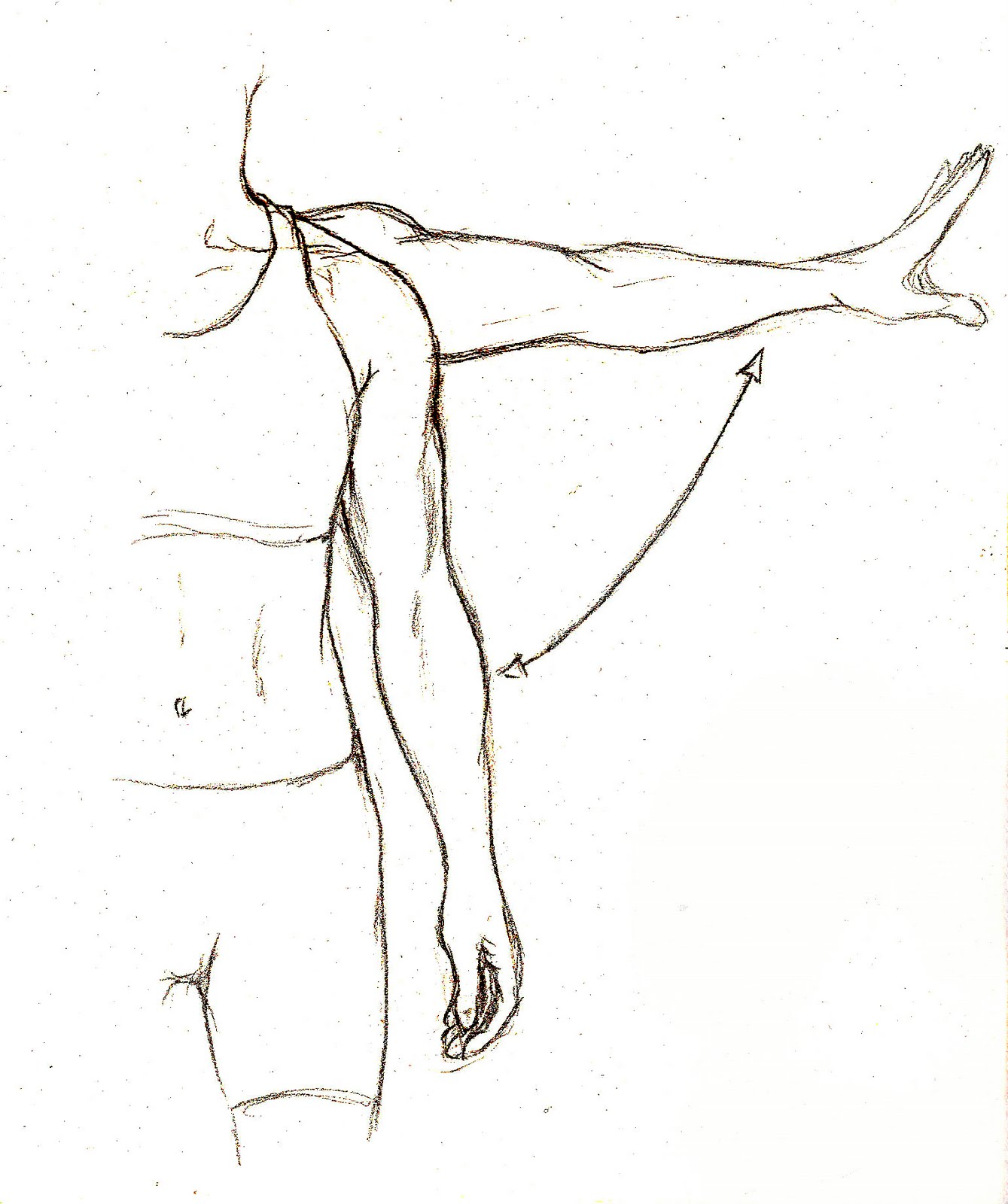
To move a part laterally, away from the midline of the body
*Supination

To rotate the forearm so that the palm faces upward
*Pronation

To rotate the forearm so that the palm faces downward
Cartilagenous Joints

a. Cartilage joins the two bones
b. Little or no movement
Synchondroses---Hyaline Cartilage

a. Epiphyseal Growth Plates/Metaphyse
b. First Sternocastal Joint(Costosternal Synchondrosis)---Cartilage connecting ribs to sternum (connection of 1st rib connecting to the sternum)
Symphyses---Fibrocartilage->(little movement)

a. Intervertebral Discs
b. Symphysis pubis
Homeostatic Imbalances of Bone
A. Osteomalacia & Rickets
B. Scurvy
C. Osteoporosis

Osteomalacia(adults) & Rickets(child)
"bo-legs"-(abnormal bone softening)
Caused by insufficient Vitamin D or Calucium. The osteoid material of bone is normal, but no calcium is added this makes the bones abnormally soft. Rickets -> Ca is not added to bone-soft bone starts to deform- especially pelvic bones, legs
*Bone fracture easily, muscle weakness, bone pain
Vit. C affects Collagen
Scurvy

Caused by insufficient Vitamin C. The collagen in the bone & in all body tissues(breaks down) is abnormal. This means the bones are full of holes, and very brittle
*Anemia, tissue ulceration & hemorrhaging poor tissue healing, gingivitis, tooth loss.

Osteoporosis
(bones with holes)
The rate of bone breakdown is faster than the rate of bone formation because osteoclast activity is abnormally high.
1. Caused by decreased ESTROGEN/Testosterone production after menopause.
2. Estrogen has a protective effect on the skeleton throughout life:
it limits the amount of bone breakdown that is caused by parathyroid hormone.
-Estrogen/testosterone- puts a break on PTH 2 make sure osteoclast activity doesn't get out of control.
3. At menopause, estrogen levels fall off drastically. The low levels of estrogen can no longer keep PTH in check-so osteoclast activity shoots up, causing bone breakdown to get out of control.
4. Other Influences- Overproduction of Parathyroid hormone, Inadequate absorption of Calcium, Inadequate intake of Calcium, Vitamins D or C.
Disorders in Skeletal GROWHT, FUNCTION, or STRUCTURE
A. Achondroplastic Dwarfism
B. Osteogenesis Imperfecta
C. Spina Bifida
D. Arthritis
Disorders in Skeletal GROWTH:
Achondroplastic Dwarfism
(abnormal hyaline cartilage)
A genetic (problem in DNA) defect where epiphyseal growth plates do not grow normally.
-Inherited, Congenital(present @ birth)
Disorders in Skeletal STRUCTURE:
Osteogenesis Imperfecta

(Brittle bone syndrome)
A genetic defect where there is insufficient or abnormal collagen synthesis. Joints are loose due to weak tendons and ligaments. The fetus often suffers fractures while still inside the utereus.
-Congenital-> abnormal collagen genes
Spina Bifida

(Can be caused by Vitamin deficiency)
Vertebral lamina fail to fuse(to form the spine) during development, leaving the spinal cord exposed. Often result in severe urinary tract problems such as under-developed organs, infection, and renal failure.
*Can be congenital or due 2 Vitamin B (folic acid)deficiency during pregnancy->bread products must have Vit. B added.
Arthritis
(Joint Inflammation)
1. Ostoarthritis-(joint replacement) 85% of arthritis cases
* Problem- erosion of the hyaline cartilage (articular)
* Age related- aging causes the cartilage 2 not repair as quickly
*New bone growth- growth spurs
*Crepitus- creaking crunching sound with movement
2. Rheumatoid Arthritis
* Problem- again hyaline cartilage erosion
* Autoimmune-WBC's attack synovial membrane-> turned into scar tissue(PANNUS)
*Joints fuse-> Ankylosis immobilized(No movement)
*Flare ups & remissions

Ostoarthritis
(joint replacement)

85% of arthritis cases
*Problem- erosion of the hyaline cartilage (articular)
*Age related- aging causes the cartilage 2 not repair as quickly
*New bone growth- growth spurs
*Crepitus- creaking crunching sound with movement
Rheumatoid Arthritis

*Problem- again hyaline cartilage erosion
*Autoimmune-WBC's attack synovial membrane-> turned into scar tissue(PANNUS)
*Joints fuse-> Ankylosis immobilized(No movement)
*Flare ups & remissions

DISORDERS of the VERTEBRAL COLUMN
1. Normal Vertebral Curvatures
2. Abnormal Curvatures
3. Problems Involving INTERVERTEBRAL DISCS
Normal Vertebral Curvatures

a. Cervical-Convex(curves toward anterior side)-Front
b. Thoracic-Concave(curves toward posterior side)-back
c. Lumbar-Convex
d. Sacral-Concave
Abnormal Curvatures
a. Kyphosis ("Hunchback")-Exaggerated thoracic(top half) curvature, as in osteoporosis
b. Lordosis ("Swayback")-Exaggerated Lumbar(lower back) curvature-Pregnant women get it temporary excessive abnormal weight, muscle length & strength in abdomen, hip Rickets
c. Scoliosis-Exaggerated lateral(from mid-line) curvature
85% of cases are idiopathic, genetic testing can predict severity of deformity, can be caused by Rickets
Kyphosis ("Hunchback")

Exaggerated thoracic(top half) curvature, as in osteoporosis
Lordosis ("Swayback")

Exaggerated Lumbar(lower back) curvature-Pregnant women get it temporary excessive abnormal weight, muscle length & strength in abdomen, hip Rickets
Scoliosis

Exaggerated lateral(from midline) curvature
85% of cases are idiopathic, genetic testing can predict severity of deformity, can be caused by Rickets
Problems Involving INTERVERTEBRAL DISCS

a. Disc Structure
(1) Annulus Fibrous-Fibrocartilage ring surrounding (2)
(2) Nucleus Pulposus- Gel-like "pulp" made largely of water
b. Herniated Discs(Ruptured) often produce SCIATICA->(pressure on sciatica nerve to leg-> numbness, paralysis pain)
The annulus fibrous weakens, causing a bulge to form or ruptures open, causing the nucleus pulposus to protrude through the opening and put pressure on spinal nerves.
Bone FRACTURES & HEALING

Classification of Fractures

HEALING of FRACTURES
1. Hematoma Formation: A Large (blood) clot forms to stop bleeding.
2. Granulation Tissue Formation(fibrocartilagenous callus): Fibroblasts create collagen fibers and blood vessels grow into the hematoma. Osteoblasts and osteoclasts move into the hematoma from the endosteum and periosteum.
3. Callus Formation:
a. A soft callus forms which includes the internal callus(btwn broken bone pieces) and External callus(bridging surface of break) areas.
b. The soft Callus(make up of granulation tissue & collagen)becomes the Hard (Bony) Callus as it is turned into spongy bone.
4. Remodeling:
Restructuring of bone continues; compact bone replaces spongy bone where appropriate.