front 1 Chemical Composition (Living Part) | back 1 1. Organic Components:
a) Osteoid- 35% of bone- soft material made of protecoglycan & collagen fibers
*Allows bone to bend/gives flexibility (resists tension/bending forces)
b) Bone Cells:
i) Osteoblasts- create/build bone by making osteoid
ii) Osteoclasts-(similar to macrophages) break down by releasing acid enzymes (work with Osteoblasts to rebuild bone).
2. Inorganic Components:
Hydroxyapatites---65% of bone->3 types calcium, mainly Ca Phosphate.
***Significance: Harden Osteoid-> responsible for hardness of bone; Helps bone resist compression (crushing forces). |
| back 2 a) Osteoid- 35% of bone- soft material made of protecoglycan & collagen fibers
* Allows bone to bend/gives flexibility (resists tension/bending forces)
b) Bone Cells--
i) Osteoblasts- create/build bone by making osteoid,
ii)Osteocytes- lose ability to make bone
iii) Osteoclasts-(similar to macrophages) uses acids & enzymes to break down bone during repair & rebuilding(remodeling) |
| back 3 35% of extracellular matrix-soft material made of proteoglycan & collagen fibers
*Allows bone to bend/gives flexibility (resists tension/bending forces) |
| back 4 *Osteoblasts- create/build bone by making osteoid, once surrounded by bone they have made, becomes osteocytes.
*Osteocytes-lose ability to make bone, maintain existing bones, uses "arms"-DENDRITIC EXTENSTIONS to send nutrients to each other.
*Osteoclasts-(similar to macrophage) uses acid & enzymes to break down bone during repair & rebuilding(remodeling).*Work with Osteoblasts to rebuild bone). |
front 5 Inorganic Components (Non-Living) | back 5 Hydroxyapatites (mineral salts)---65% of extracellular matrix->3 types of calcium, mainly Ca Phosphate.
***Significance:Hardens bone tissue, Osteoid-> responsible for hardness of bone; Helps bone resist compression (crushing forces). |
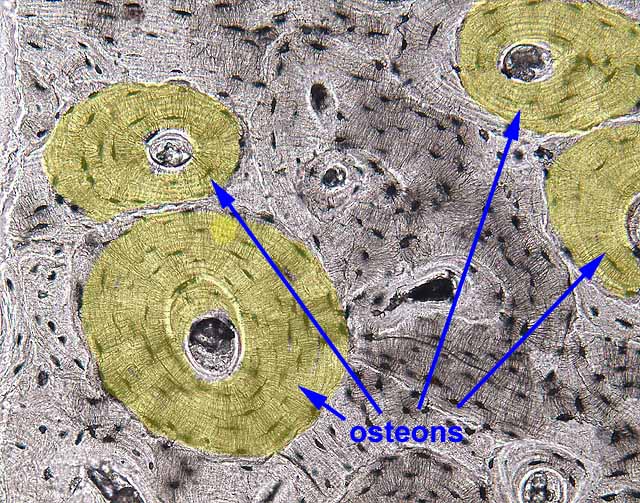
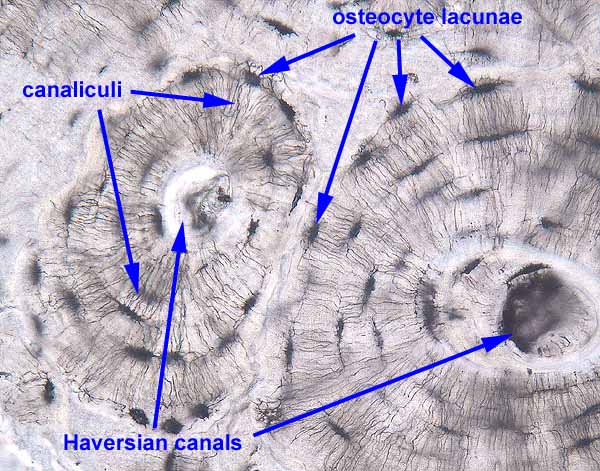
front 6 Organization of bone matrix | back 6 1. The matrix is organized into layers of bone called lamellae <-(layers)
a.) In compact bone(designed to with stand stress from one direction), there are three types of lamellae:
*Osteons (concentric lamellae)
*Interstitial Lamellae-(incomplete layers) fragments/pieces of old osteons formed during remodeling.
*Circumferntial Lamellae- bony layer that underlies the perisotem or endosteum.
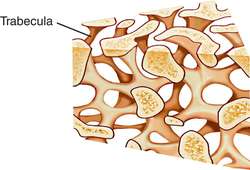
b.) In cancellous/spongy bone, the lamellae form trabeculae, or narrow branches that connect together to form a loose web or net structure. *Can bear stress from multiple different directions |
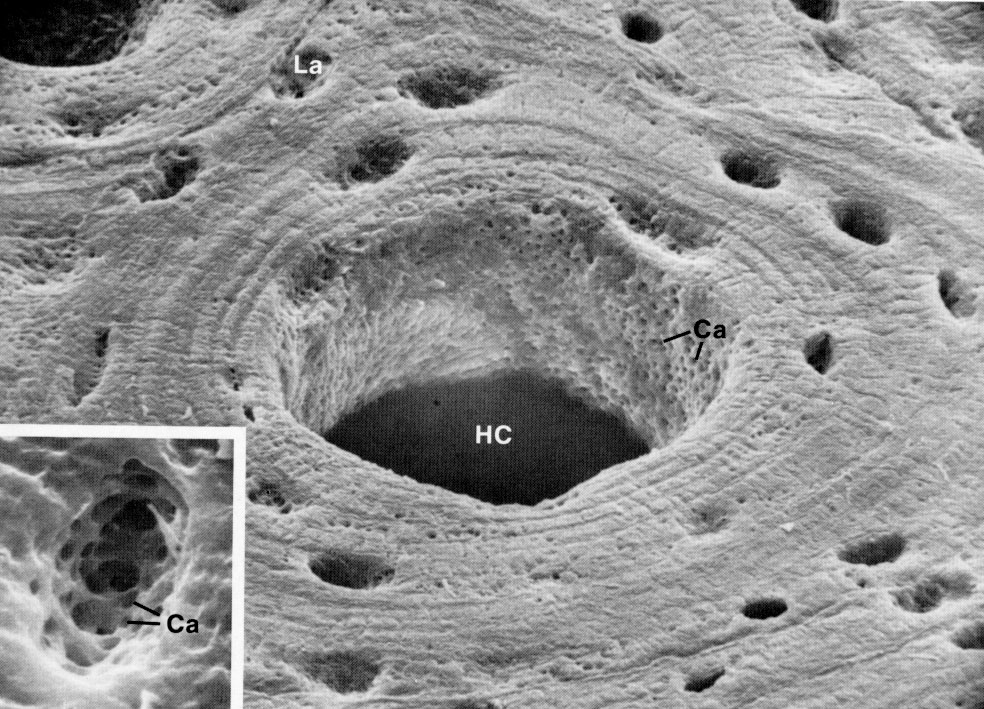
front 7 organization of bone matrix con... | back 7 2. Within the matrix of both (compact and cancellous bone) osteocytes are found in holes called Lacunae. The dendritic extensions<-(branching) of each osteocyte are found in tiny crack-like passageways called canaliculi.
3. Blood vessels and nerves are found in Haversian/Central Canals, located in the center of osteons (parallel to bone shaft), and in Perforating/Volkmann's Canals (perpendicular or transverse to bone shaft). |
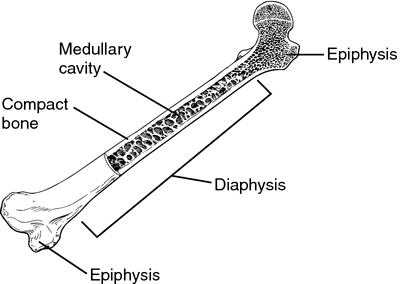
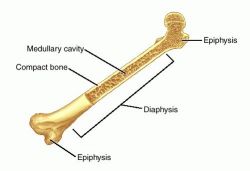
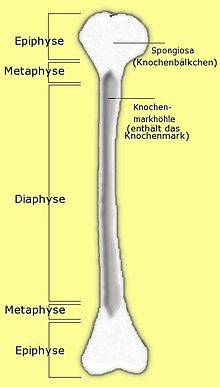
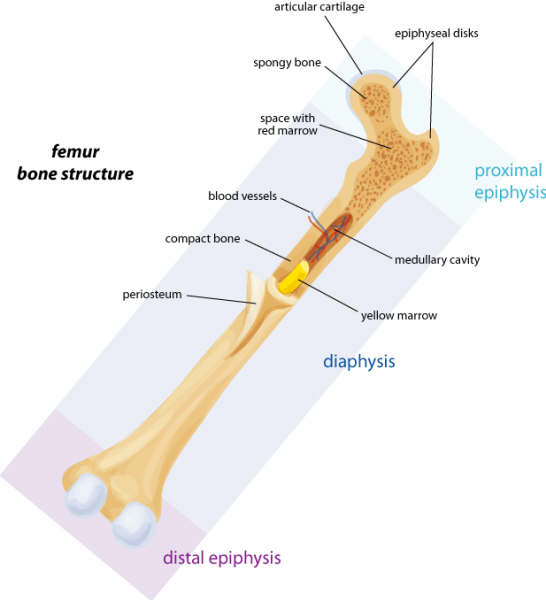
| back 8 A. Diaphysis
B. Epiphysis
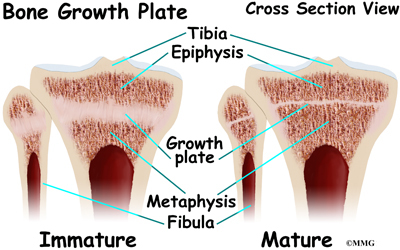
C. Metaphysis/Growth Plate
D. Articulation
E. Medullary Cavity (Bone Marrow Cavity)
F. Periosteum |
| back 9 The hollow shaft made of compact bone |
| back 10 The round ends, filled with spongy bone and covered by outer layer of compact bone |
| back 11 Band of hyaline cartilage, area located between diaphysis and epiphysis. Before puberty contains the epiphyseal growth plate. After puberty, when the growth plate disappears, contains the epiphyseal line (scar where growth plate was).
*allows for growth in bone length |
| back 12 Where two or more bones come together to form a joint |
front 13 Medullary Cavity (Bone Marrow Cavity) | back 13 1. Red Bone Marrow/Myeloid Tissue-(Reticular C.T.) The birthplace of RBC's and WBC's; Located throughout skeleton of children but only in select locations of adult skeleton.
Major-Pelvic bone, Top epiphyes of femor, humerous.
Miner locations; Vertabrae, ribs, skull
2. Yellow Bone Marrow- Primarily adipose (fat) tissue; Most myeloid tissue turns into this.
3. Endosteum (inside)--Membrane made of a single layer of osteoblasts and osteoclasts which lines the medullary cavity and covers trabeculae of spongy bone' Essential because it provides bone cells needed for growth, remodeling, and repair of bone. |
| back 14 Covers outer surface of bones
1. Outer Layer--Dense irregular collagenous tissue; important because tendons (& therefore muscle) attach to this tissue. Sharpey's fibers (perforating fibers) attach the periosteum to tendons and ligaments, forming strong connections to them.
2. Inner layer--Single layer of osteoblast; Essential because it provides bone cells needed for bone growth, remodeling, and repair. |
front 15 Formation of Bone in the Early Skeleton | back 15 Overview
The skeleton of a human embryo is made of two tissues that will gradually be turned into bone. The process of making bone is called ossification.-->formation of bone |
front 16 Intramembranous ossification | back 16 *Forms bone from a soft membrane (tissue) made of collagen (similar to dense/fiborus tissue) called MESENCHYME, (embryonic tissue)
*Forms flat bones of skull, & Clavicles
*Process complete by age 2 |
front 17 Endochondral ossification | back 17 *Forms bones from hyaline cartilage;(Hyaline remains in growth plates after birth)--> allow skeleton to grow in length.
*Forms rest of skeleton
*Process complete by end of puberty |
front 18 Intramembranous ossification Steps | back 18 All of the flat skull bones and the clavicles are made from a fiborous connective tissue called mesenchyme.
STEP 1: Ossification centers (REGIONS OF BONE FORMATION) appear in the mesenchyme.(area where bones beginning to be made-osteoblast)
a.) Osteoblast cells produce the bone matrix, or osteoid.
*b.) Spongy bone, or woven bone, grows and expands as a series of trabeculae that grow outward freom the ossification centers.
c.) Blood vessels grow into the woven bone as it forms. |
front 19 Intramembranous ossification Steps con... | back 19 STEP 2: The periosteum forms on the surface of the bone.
*provides the osteoblast on the surface so the next step can happen.
STEP 3: Compact bone(AkA Bony Collar->surface layer) forms beneath the periosteum.
STEP 4: Blood vessels inside the bone turn into Red bone marrow.
***The skull bones are not fully ossified (turned into bone) at birth. They become ossified around age 2. Until then, the parts of these bones which are still mesenchyme are called FONTANELS or "soft spots" |
front 20 Endochondral ossification IN THE FETUS | back 20 All other bones are formed from an entirely different tissue--hyaline cartilage.
STEP 1: cartilage occurs by TWO METHODS:
a. Appositional Growth--cartilage cells on surface of the existing cartilage multiply and produce matrix. causing growth of the cartilage on its surface.
b. Interstitial Growth--Cartilage cells in the center of the existiong cartilage multiply and produce matrix, causing growth of the cartilage from within.(in btwn)
STEP 2: The periosteum forms on the surface of the cartilage.
STEP 3: Compact bone forms beneath the periosteum.
STEP 4: Calcification and cavitation occur in the center of the cartilage.
Hypertrophy of the chondrocytes occurs before this step begins. the cartilage cells enlarge before they add calcium carbonate to the cartilage. causing their own death and therefore creating holes (cavities) in the cartilage. Adding calcium to the cartilage kills it so that it can be replaced with bone. |
front 21 Endochondral ossification IN THE FETUS con... | back 21 STEP 5: Primary Ossicfication Centers appear.
a.The periosteal bud invades the cavities and spongy bone forms. The bud, a blood vessel, grows into the hole in the center of the cartilage, bringing along with it osteoblasts that will start primary ossification centers. These centers will produce spongy bone in the diaphysis (shaft)
b. The diaphysis elongates, thinkens, and a medullary cavity forms.
STEP 6: Secondary Ossification Centers appear.Shortly before or after birth, these centers develop and turn the cartilage of the epiphyses into spongy bone. At birth, hyaline cartilage remains at only two locations.
1.) Growth plates-metaphyses
2.) On the surface of the epiphyses, called articular cartilage. |
| back 22 1. Bone is organized into layers called lamellae.
a) In compact bone, the lamellae form circular patterns: Osteons (Concentric lamellae) -->Target pattern-> made of circular rings.
*Designed to with stand stress from one direction
b) In cancellour/spongy bone, the lamellae from trabeculae, or narrow branches that connect together to form a loose web or net structure.
2. Blood vessels and nerves are found in Haversian Canals, located in the center of osteons, and in Perforating/Volkmann's Canals which lie at right angles to the Haversian Canals. in same direction as bone shaft. (parallel) |
| back 23 There are three types of lamellae:
*Osteons (concentric lamellae)- Target patterns-> made of circular rings
*Interstitial Lamellae-(incomplete layers)-> fragments/pieces of old osteons formed during remodeling.
*Circumferntial Lamellae- bony layer that underlies the perisotem or endosteum.
--Designed to with stand stress from one direction |
| back 24 The lamellae form trabeculae, or narrow branches that connect together to form a loose web or net structure. *Can bear stress from multiple different directions |
front 25 BONE GROWTH IN LENGTH in the GROWTH PLATES | back 25 The long bones of the skeleton can grow in length up until 18-21 years of age because endochondral ossification occurs within the growth plates during that time.
The steps in the formation of bone can be seen in the CELL LAYERS OF THE GROWTH PLATES (METAPHYSES):
1) Zone of Resting or Reserve Cartilage (nearest to epiphysis)
2) Zone of Proliferation-Cartilage growth
3) Zone of Hypertrophy
4) Zone of Calcification |
| back 26 Besides growing in length, bones must also grow in diameter in the young adult. Growth in diameter is accomplished by growth of the actual bone, NOT by growth of the cartilage in the growth plate (metaphysis).
Bone has appositional growth but NOT interstitial grwoth
*1.) Can't expand from within b/c it is calcified (harden).
*2.) Bone can only be added to surfaces (inside & outside) b/c osteoblasts are...not found in shaft, only on outer surface (periosteum) & inner surface (endosteum). |
| back 27 IN GENERAL:
The simultaneous break down (reabsorption) by osteoclast & rebuilding (depostion) by osteoclast.These processes should occur @ equal rates. (or u'll end up with osteoporosis)
*1/5 of skeleton is remodeled every yr. Epiphyses (ends) of femur are most frequently rebuilt, is dependent upon levels of activity' creates interstitial lamellae. |
| back 28 A. To adjust bone to stress- is slight bending of bone caused by skeletal muscle contraction.Causes tiny electrical charges (currents) that "tell" the bone cells how to remodel.
B. To increase Length and Diameter of Medullary Cavity as bone grows |
front 29 PURPOSES for Remodeling con... | back 29 C. To Regulate Calcium levels in the body
Ca is crucial for:
*proper electricity in nerves & brain
*proper organ functions
*proper skeletal & Cardiac muscle construction
*proper blood clothing |
front 30 Calcium Homeostasis (How bone regulates Ca levels)
(Keeping Calcium @ steady level) | back 30 A. Roles of Osteoblasts and Osteoclasts
1. Osteoblasts create new bone and in the process cause calcium to deposited in the bone because it leaves the bloodstream and enters the forming bone. Thus, they reduce/lower calcium levels in the blood.
2. Osteoclasts break down bone and in the process cause calcium to be released from the bone. Thus, they increase/raise calcium levels in the blood. |
| back 31 1. Parathyroid Hormone (PTH)--Its job is to prevent hypocalcemia (too LITTLE calcium)
*Most important of the 2 hormones b/c low Ca is deadly-> it causes skeletal muscle spasms & paralysis-> death by asphyxiation.
PTH raises calcium levels in THREE ways:
a. Effect on the Intestines
b. Effect on Kidneys
c. Effect on Bone |
front 32 Influence of Hormones
PTH raises calcium levels in THREE ways:
Effect on the INTESTINES | back 32 --> Getting Ca from food
1) This effect is PTH's way of increasing the body's natural process that brings Ca into the body/blood. PTH increases the absorption of calcium by the intestines.
2) This action is reinforced by one of PTH's effects on the kidneys. |
front 33 Influence of Hormones
PTH raises calcium levels in THREE ways:
Effect on the KIDNEYS | back 33 ->lose with kidneys by uren
1) The first effect is PTH's way of decreasing any natural process that causes Ca loss in body: PTH decreases urinary loss of calcium by the kidneys, called calcium excretion.
2) The second effect on the kidneys helps the INTESTINES absorb calcium; PTH increases Vitamin D produciton by the kidneys. Without enough Vitamin D, the intestines can't bring calcium into the body-it's an essential part of the process. |
front 34 Influence of Hormones
PTH raises calcium levels in THREE ways:
Effect on BONE | back 34 1) This effect is PTH's way of releasing stored Ca (in bones) in the body that has a surplus of it: PTH causes the bones to release calcium.
2) To do this, PTH increases osteoclasts activity (bone breakdown) because the only way bones can release their extra store of calcium is to dissolve them.
Only 1% Ca in bone is available for release-called exchangeable Ca |
front 35 Influence of Hormones
Calcitonin Hormone | back 35 It's job is to prevent hypercalcemia (too MUCH calcium)--> more rare, rarely leads to death
strange hormone b/c it's not very good at it's job.
*Calcitonin levels are high only in children, (for growth of skeleton) except during pregnancy--> levels rise to protect mom's bones.
Lowers Calcium levels in TWO ways:
Major action: Decrease Osteoclast activity
Weak secondary action: Increase osteoblast activity |
front 36 Influence of Hormones
Calcitonin Hormone-
Lowers Calcium levels in TWO ways:Major action | back 36 *Major action: Decrease(slows down) Osteoclast activity (bone breakdown) to stop the release of calcium from bones. (If calcium levels are high, there doesn't need to be extra calcium coming out of the bones). |
front 37 Influence of Hormones
Calcitonin Hormone-
Lowers Calcium levels in TWO ways:Weak secondary action | back 37 Weak secondary action: Increase osteoblast activity (bone building). As new bone is made, calcium is pulled into the bones to harden them, which lowers calcium levels in the blood.
*used as treatment for osteoporosis- but still not highly effective |
front 38 Articulations and their Movements | back 38 A. Major Types Of Movement:
1. Flexion & Extension
2. Abduction & Adduction
3. Supination & Pronation
B. Articulations
1. Fibrous Joints
2. Cartilagenous Joints
3. Synovial Joints |
| back 39 1.) General Description
a. Small (usually) ligaments join the two bones
b. No movement--synarthrotic-->(together Joint)
2.) Sutures--Seams between skull bones(which are attached via tiny ligaments)
3.) Syndesmoses---Joint in the gap between radius & ulna, tibia & fibula
4.) Gomphoses---Joint between the teeth and teeth sockets-Nail shape |
| back 40 1.) Synchondroses---Hyaline Cartilage-(btwn bones)-Synarthrotic No movement
a.) Epiphyseal Growth Plates
b.) First Sternocostal Joint--1st rib's connection(via costal cartilage) to sternum
Synostoses-joint where 2 or more bones fuse into one bone/piece EX: Growth plates/Sutures |
front 41 CARTILAGENOUS JOINTS con... | back 41 2.) Symphyses---Fibrocartilage *amphiarthrothic-"btwn joint" limited movement
a. Intervertebral Discs-pads btwn
b. Symphysis Pubis
c. Sternal Angle |
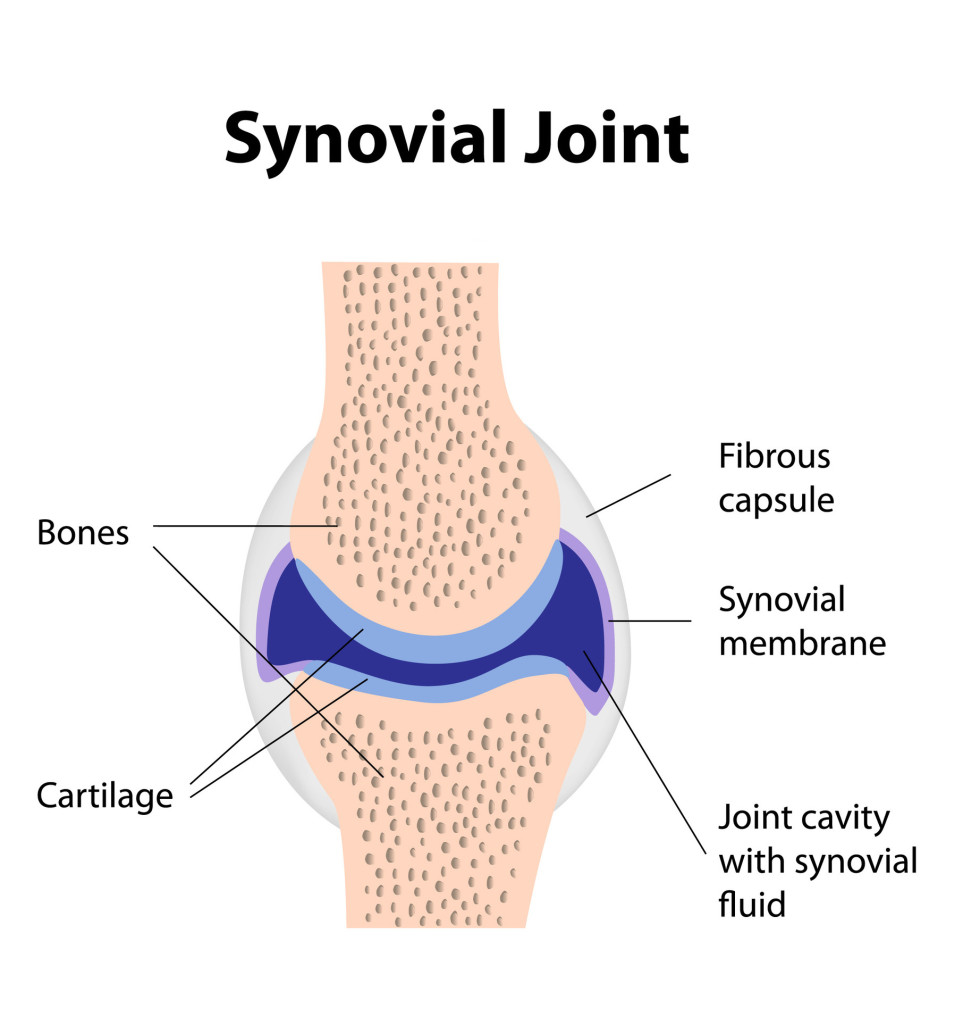
| back 42 *Has cartilage(articular) hyaline also but it moves
General Description
a. Allows for Free Movement-diarthrotic
b. Contain a Joint Cavity-A space between the bones, created by a joint capsule(inner layer) and filled with synovial fluid(synovial membrane)
c. Contain Large Ligaments
d. Contain Bursae-"Sacks" of fluid-filled synovial membrane located where tendons and ligaments rub against bone-> Protects tendons & ligaments
e. Contain Articular Cartilage--Hyaline cartilage on epiphyseal bone surfaces where bones make contact/rub together
f. May Contain Menisci--Disc of fibrocartilage that floats between the bones of the knee joint |
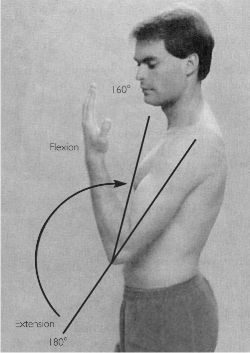
| back 43 A. Flextion & Extension
B. Abduction & Adduction
C. Supination & Pronation |
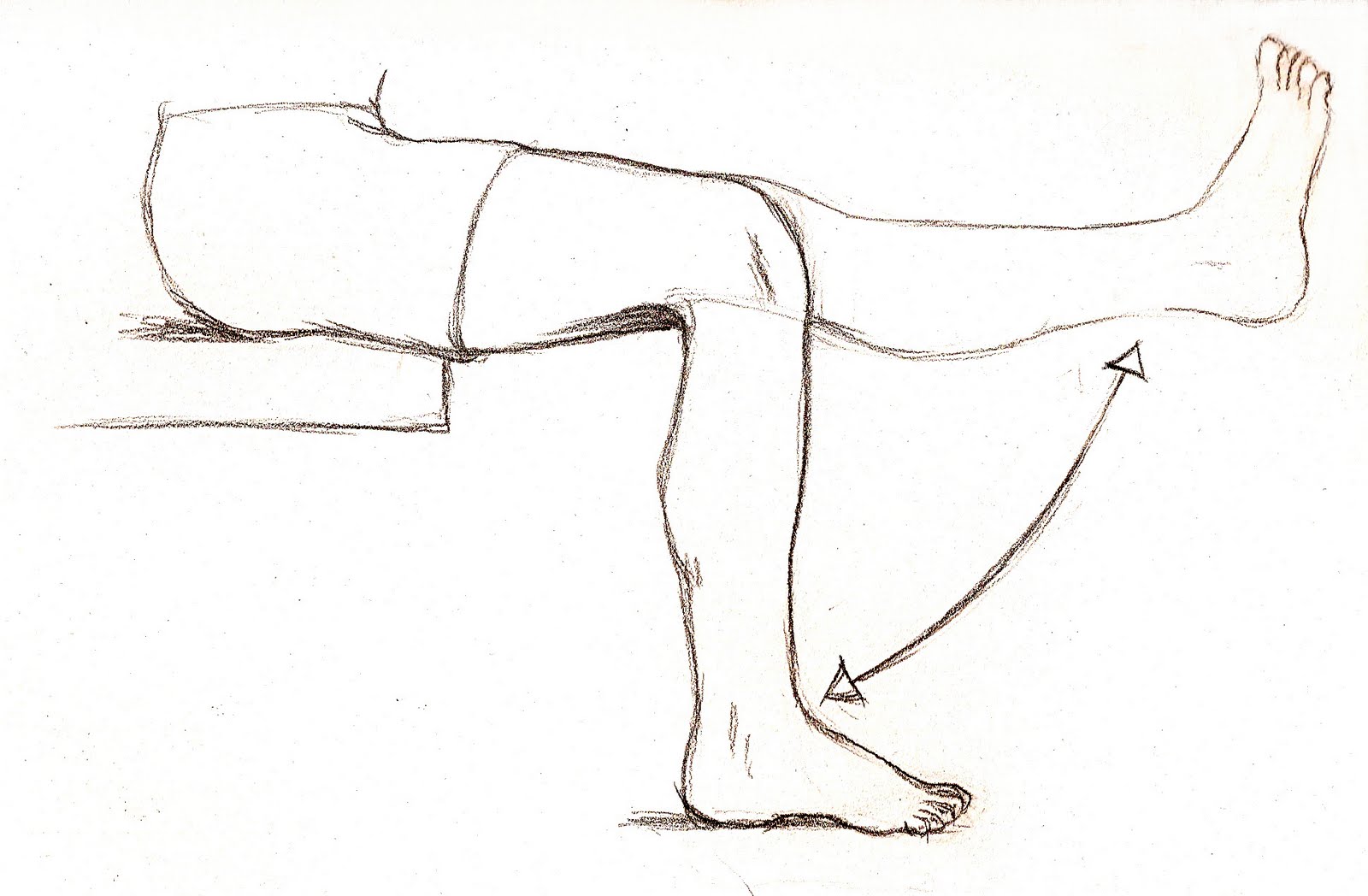
front 44 Flexion, Extension & Hyperextension | back 44 Flexion= To bend a limb; also an anterior movement-Forwards
Extention= To straighten a limb; Also a movement that returns the body part to the anatomical position; Also a posterior movement-backwards
Hyperextesion= Movement behind/posterior to anatomical position.
Ex: looking up, bending backwards at waist.Moving arm or leg behind the body. |
| back 45 To bend a limb; also an anterior movement-Forwards |
| back 46 To straighten a limb; Also a movement that returns the body part to the anatomical position; Also a posterior movement-backwards |
| back 47 Movement behind/posterior to anatomical position.
Ex: looking up, bending backwards at waist.Moving arm or leg behind the body. |
| back 48 Abduction= To move a part laterally, away from the midline of the body-OUTWARD
Adduction= To move a part medially, toward the midline of the body-INWARD |
| back 49 To move a part laterally, away from the midline of the body-OUTWARD |
| back 50 To move a part medially, toward the midline of the body-INWARD |
| back 51 Supination= To rotate the forearm so that the palm faces upward
Pronation= To rotate the forearm so that the palm faces downward |
| back 52 To rotate the forearm so that the palm faces upward |
| back 53 To rotate the forearm so that the palm faces downward |
| back 54 1. General description:
a. Allows for Free Movement-->diarthrotic
b. Contain a Joint Cavity---A space between the bones, created by a joint capsule (Inner layer) and filled with synovial fluid,(synovial membrane).
c. Contain large ligaments
d. Contain Bursa---A "Sacks" of fluid-filled synovial membrane located where tendons and ligaments rub against bone (cushioning)-proteccts tendons & ligaments from damage(rubbing).
e. Contain Articular Cartilage--Hyaline cartilage on epiphyseal bone surfaces where bones can make contact/rub together
f. May Contain Menisci--Disc of fibrocartilage that floats btwn the bones of the knee joint |
| back 55 a. Plane/Gliding Joint---Two flat articulating bone surfaces
> Nonaxial Movement: Small slipping or gliding movements only-least movement of all synovial types.
*1) Intercarpal Joints (between wrist bones)
2) Sternoclavicular joint (btwn sternum & clavicle)
*3) Intervertebral joints (btwn articular processes of vertebrae)
4)Sacroiliac Joint (btwn sacrum and iliac bones)
b. Hinge Joint---Rounded process of one bone fits into concave surface of other bone-Door movements (front 2 back)
>Uniaxial Movement:-> Movement in one plane (axis)-allows flexion & extention (front 2 back) only
1) Knee joint
*2) Elbow Joint-(btwn Humerous & ulna)
3) Interphalangeal joints (btwn finger & toe bones) |
front 56 Types of Synovial Joints, Cont...1 | back 56 c.Pivot Joint(half-rotation)--- One bone has a round process that is held by a ring ligament to the 2nd bone; allowing first bone to rotates
>Uniaxial Movement:Rotation back & forth in one plane (axis)
1) Atlanoaxial joint(2nd neck joint; btwn atlas & axis, first two cervical vertebrae)
2)Elbow joint (btwn head of radius & ulna--allows for rotation of the forearm)
*Both uniaxial types are in elbow.
d. Saddle Joint---One bone surface is concave(curves towards back) while the other is convex (curves forward)
Biaxial Movement: Movement in two planes-Front 2 Back (flexion & extension) & side 2 side (abduction & adduction)
**Thumb Joint: (1st carpometacarpal joint) |
front 57 Types of Synovial Joints, Cont...2 | back 57 e. Ball & Socket---Round bone process fits into indention of second bone
> Triaxial/Multiaxial Movement:Movement in three planes, one of which is rotation (has most movement of all synovial types).
**Shoulder and hip joints
f. Ellipsoid/Condyloid(oval shaped)---Modified ball and socket where "ball" is oval rather than round
> Biaxial Movement: Movement in two planes
1) Atlanto-occipital joint (1st neck joint btwn occipital condyles and atlas)
2) Knuckles (btwn metacarpals and phalanges)
3) Btwn radius & carpals at wrist |
front 58 Type of Synovial Joint: Plane/Gliding | back 58 Two flat articulating bone surfaces
> Nonaxial Movement: Small slipping or gliding movements only-least movement of all synovial types.
*1) Intercarpal Joints (between wrist bones)
2) Sternoclavicular joint (btwn sternum & clavicle)
*3) Intervertebral joints (btwn articular processes of vertebrae)
4)Sacroiliac Joint (btwn sacrum and iliac bones) |
front 59 Type of Synovial Joint: Hinge Joint | back 59 Rounded process of one bone fits into concave surface of other bone-Door movements (front 2 back)
>Uniaxial Movement:-> Movement in one plane (axis)-allows flexion & extention (front 2 back) only
1) Knee joint
*2) Elbow Joint-(btwn Humerous & ulna)
3) Interphalangeal joints (btwn finger & toe bones) |
front 60 Type of Synovial Joint: Pivot Joint | back 60 One bone has a round process that is held by a ring ligament to the 2nd bone; allowing first bone to rotates
>Uniaxial Movement:Rotation back & forth in one plane (axis)
1) Atlanoaxial joint(2nd neck joint; btwn atlas & axis, first two cervical vertebrae)
2)Elbow joint (btwn head of radius & ulna--allows for rotation of the forearm)
*Both uniaxial types are in elbow. |
front 61 Type of Synovial Joint: Saddle Joint | back 61 One bone surface is concave(curves towards back) while the other is convex (curves forward)
>Biaxial Movement: Movement in two planes-Front 2 Back (flexion & extension) & side 2 side (abduction & adduction)
**Thumb Joint: (1st carpometacarpal joint) |
front 62 Type of Synovial Joint:Ball & Socket | back 62 Round bone process fits into indention of second bone
> Triaxial/Multiaxial Movement:Movement in three planes, one of which is rotation (has most movement of all synovial types).
**Shoulder and hip joints |
front 63 Type of Synovial Joint:Ellipsoid/Condyloid | back 63 (oval shaped)---Modified ball and socket where "ball" is oval rather than round
> Biaxial Movement: Movement in two planes
1) Atlanto-occipital joint (1st neck joint btwn occipital condyles and atlas)
2) Knuckles (btwn metacarpals and phalanges)
3) Btwn radius & carpals at wrist |
front 64 Osteons(Concentric lamellae) | back 64 Target pattern-> made of circular rings
*Designed to withstand stress form one direction |
| back 65 (Incomplete layers)-Fragments/pieces of old osteons formed during remodeling. |
| back 66 bony layer that underlies the periostem or endosteum. |
| back 67 The lamellae form trabeculae or narrow branches that connect together to form a loose web or net structure.
*Can bear stress from multiple different directions |
| back 68 Blood vessels & nerves are found here, Located in the center of osteons (parallel to bone shaft), & in Perforating/ Volkmann's Canals (perpendicular or transverse to bone shaft) |
| back 69 Holes within the matrix of both (compact & cancellous bone) where osteocytes are found. |
| back 70 Tiny crack-like passageways where the dendritic extentions of each osteocyte are found. |
| |
| back 72 The hollow shaft made of compact bone |
| back 73 Rounded ends,filled with spongy bone and covered by outer layer of compact bone |
| back 74 Band of hyaline cartilage, area located between diaphysis and epiphysis. Before puberty contains the epiphyseal growth plate. After puberty, when the growth plate disappears, contains the epiphyseal line (scar where growth plate was).
*allows for growth in bone length |
| back 75 Where two or more bones come together to form a joint. |
| back 76 (Bone Marrow Cavity)
1. Red Bone Marrow/Myeloid Tisssue(reticular C.T.)- the birthplace of RBC's and WBC's; Located throughout skeleton of children but only in select locations of adult skeleton.
Location in adults; Major:pelvic bone, top epiphyes of humerus,femur; Minor locations; vertabrae, ribs, skull
2. Yellow Bone Marrow Primarily fat tissue; Most myeloid tissue turns into this. |
| back 77 Seams between skull bones (which are attached via tiny ligaments) |
front 78 Fibrous Joint: Syndesmosis | back 78 Joints between tibia & fibula and between radius & ulna |
| back 79 To bend a limb; also an anterior movement |
| back 80 To straighten a limb; Also a movement that returns the body part to the anatomical position; Also a posterior movement |
| back 81 To move a part laterally, away from the midline of the body |
| back 82 To rotate the forearm so that the palm faces upward |
| back 83 To rotate the forearm so that the palm faces downward |
| back 84 a. Cartilage joins the two bones
b. Little or no movement |
front 85 Synchondroses---Hyaline Cartilage | back 85 a. Epiphyseal Growth Plates/Metaphyse
b. First Sternocastal Joint(Costosternal Synchondrosis)---Cartilage connecting ribs to sternum (connection of 1st rib connecting to the sternum) |
front 86 Symphyses---Fibrocartilage->(little movement) | back 86 a. Intervertebral Discs
b. Symphysis pubis |
front 87 Homeostatic Imbalances of Bone | back 87 A. Osteomalacia & Rickets
B. Scurvy
C. Osteoporosis |
front 88 Osteomalacia(adults) & Rickets(child) | back 88 "bo-legs"-(abnormal bone softening)
Caused by insufficient Vitamin D or Calucium. The osteoid material of bone is normal, but no calcium is added this makes the bones abnormally soft. Rickets -> Ca is not added to bone-soft bone starts to deform- especially pelvic bones, legs
*Bone fracture easily, muscle weakness, bone pain
Vit. C affects Collagen |
| back 89 Caused by insufficient Vitamin C. The collagen in the bone & in all body tissues(breaks down) is abnormal. This means the bones are full of holes, and very brittle
*Anemia, tissue ulceration & hemorrhaging poor tissue healing, gingivitis, tooth loss. |
front 90 Osteoporosis
(bones with holes) | back 90 The rate of bone breakdown is faster than the rate of bone formation because osteoclast activity is abnormally high.
1. Caused by decreased ESTROGEN/Testosterone production after menopause.
2. Estrogen has a protective effect on the skeleton throughout life:
it limits the amount of bone breakdown that is caused by parathyroid hormone.
-Estrogen/testosterone- puts a break on PTH 2 make sure osteoclast activity doesn't get out of control.
3. At menopause, estrogen levels fall off drastically. The low levels of estrogen can no longer keep PTH in check-so osteoclast activity shoots up, causing bone breakdown to get out of control.
4. Other Influences- Overproduction of Parathyroid hormone, Inadequate absorption of Calcium, Inadequate intake of Calcium, Vitamins D or C. |
front 91 Disorders in Skeletal GROWHT, FUNCTION, or STRUCTURE | back 91 A. Achondroplastic Dwarfism
B. Osteogenesis Imperfecta
C. Spina Bifida
D. Arthritis |
front 92 Disorders in Skeletal GROWTH:
Achondroplastic Dwarfism
(abnormal hyaline cartilage) | back 92 A genetic (problem in DNA) defect where epiphyseal growth plates do not grow normally.
-Inherited, Congenital(present @ birth) |
front 93 Disorders in Skeletal STRUCTURE:
Osteogenesis Imperfecta | back 93 (Brittle bone syndrome)
A genetic defect where there is insufficient or abnormal collagen synthesis. Joints are loose due to weak tendons and ligaments. The fetus often suffers fractures while still inside the utereus.
-Congenital-> abnormal collagen genes |
| back 94 (Can be caused by Vitamin deficiency)
Vertebral lamina fail to fuse(to form the spine) during development, leaving the spinal cord exposed. Often result in severe urinary tract problems such as under-developed organs, infection, and renal failure.
*Can be congenital or due 2 Vitamin B (folic acid)deficiency during pregnancy->bread products must have Vit. B added. |
front 95 Arthritis
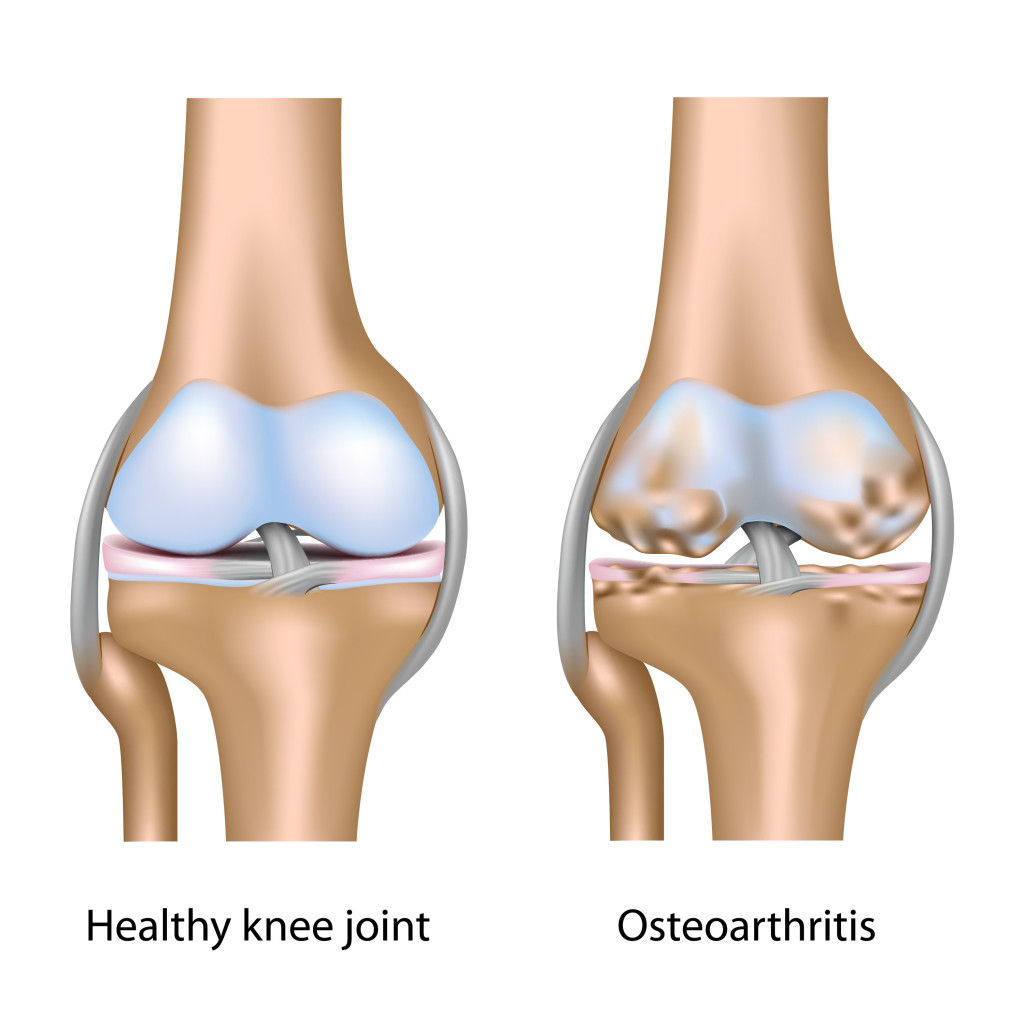
(Joint Inflammation) | back 95 1. Ostoarthritis-(joint replacement) 85% of arthritis cases
* Problem- erosion of the hyaline cartilage (articular)
* Age related- aging causes the cartilage 2 not repair as quickly
*New bone growth- growth spurs
*Crepitus- creaking crunching sound with movement
2. Rheumatoid Arthritis
* Problem- again hyaline cartilage erosion
* Autoimmune-WBC's attack synovial membrane-> turned into scar tissue(PANNUS)
*Joints fuse-> Ankylosis immobilized(No movement)
*Flare ups & remissions |
front 96 Ostoarthritis
(joint replacement) | back 96 85% of arthritis cases
*Problem- erosion of the hyaline cartilage (articular)
*Age related- aging causes the cartilage 2 not repair as quickly
*New bone growth- growth spurs
*Crepitus- creaking crunching sound with movement |
| back 97 *Problem- again hyaline cartilage erosion
*Autoimmune-WBC's attack synovial membrane-> turned into scar tissue(PANNUS)
*Joints fuse-> Ankylosis immobilized(No movement)
*Flare ups & remissions |
front 98 DISORDERS of the VERTEBRAL COLUMN | back 98 1. Normal Vertebral Curvatures
2. Abnormal Curvatures
3. Problems Involving INTERVERTEBRAL DISCS |
front 99 Normal Vertebral Curvatures | back 99 a. Cervical-Convex(curves toward anterior side)-Front
b. Thoracic-Concave(curves toward posterior side)-back
c. Lumbar-Convex
d. Sacral-Concave |
| back 100 a. Kyphosis ("Hunchback")-Exaggerated thoracic(top half) curvature, as in osteoporosis
b. Lordosis ("Swayback")-Exaggerated Lumbar(lower back) curvature-Pregnant women get it temporary excessive abnormal weight, muscle length & strength in abdomen, hip Rickets
c. Scoliosis-Exaggerated lateral(from mid-line) curvature
85% of cases are idiopathic, genetic testing can predict severity of deformity, can be caused by Rickets |
| back 101 Exaggerated thoracic(top half) curvature, as in osteoporosis |
| back 102 Exaggerated Lumbar(lower back) curvature-Pregnant women get it temporary excessive abnormal weight, muscle length & strength in abdomen, hip Rickets |
| back 103 Exaggerated lateral(from midline) curvature
85% of cases are idiopathic, genetic testing can predict severity of deformity, can be caused by Rickets |
front 104 Problems Involving INTERVERTEBRAL DISCS | back 104 a. Disc Structure
(1) Annulus Fibrous-Fibrocartilage ring surrounding (2)
(2) Nucleus Pulposus- Gel-like "pulp" made largely of water
b. Herniated Discs(Ruptured) often produce SCIATICA->(pressure on sciatica nerve to leg-> numbness, paralysis pain)
The annulus fibrous weakens, causing a bulge to form or ruptures open, causing the nucleus pulposus to protrude through the opening and put pressure on spinal nerves. |
| |
front 106 Classification of Fractures | |
| back 107 1. Hematoma Formation: A Large (blood) clot forms to stop bleeding.
2. Granulation Tissue Formation(fibrocartilagenous callus): Fibroblasts create collagen fibers and blood vessels grow into the hematoma. Osteoblasts and osteoclasts move into the hematoma from the endosteum and periosteum.
3. Callus Formation:
a. A soft callus forms which includes the internal callus(btwn broken bone pieces) and External callus(bridging surface of break) areas.
b. The soft Callus(make up of granulation tissue & collagen)becomes the Hard (Bony) Callus as it is turned into spongy bone.
4. Remodeling:
Restructuring of bone continues; compact bone replaces spongy bone where appropriate. |