Microbiology Chapter 16
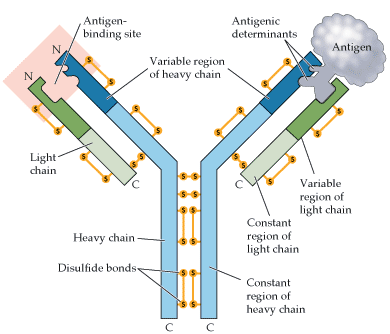
What is an antibody?
(immunoglobulin) Proteinaceous antigen-binding molecule secreted by plasma cells.
What is an antigen? Distinguish between epitope and antigen
antigen: foreign material
epitope: the specific regions on an antigen recognized by specific antigen receptors, that is, the part of the antigen that fits into the antigen binding site of the antigen receptor.
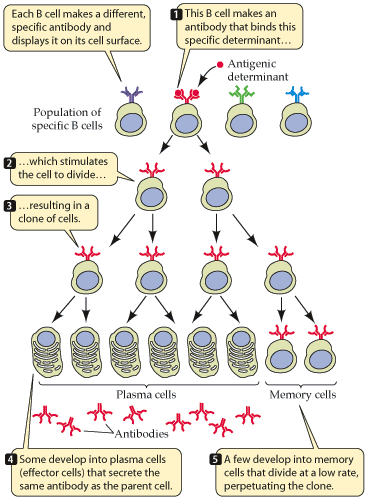
What is the process that stimulates B cell proliferation and differentiation to plasma cells? (clonal selection mechanism)
- Millions of different B cells exist, each with a different, specific antibody which they display on their cell surface.
- If a person is exposed to an antigen then the B cell with the matching antibody will be stimulated to divide.
- This
results in a clone of cells (hence the term
“clonal selection”):
- Some become
plasma cells.
- These are called effector cells because they simply secrete the antibodies that bind to the antigen (i.e. effector antibodies).
- They are antibody factories.
- Some become memory
cells.
- These stay around to provide protection for a future exposure to this antigen.
- In the future, instead of having just one B cell to respond there will be many.
- Some become
plasma cells.
What are the different mechanisms that antibodies contribute to immunity?
Effectors:
- Effector antibodies circulate in the blood system.
- They neutralize poisonous antigens and destroy microbes that bear antigens
Receptors:
- The stem of the antibody is attached to the plasma membrane of a B cell.
- Two arms search the blood and lymph for antigens.
- The binding of an antigen to receptor antibodies triggers responses in the cells that bear antibodies.
What are cytokines?
Proteins secreted by many types of cells that regulate adaptive immune responses
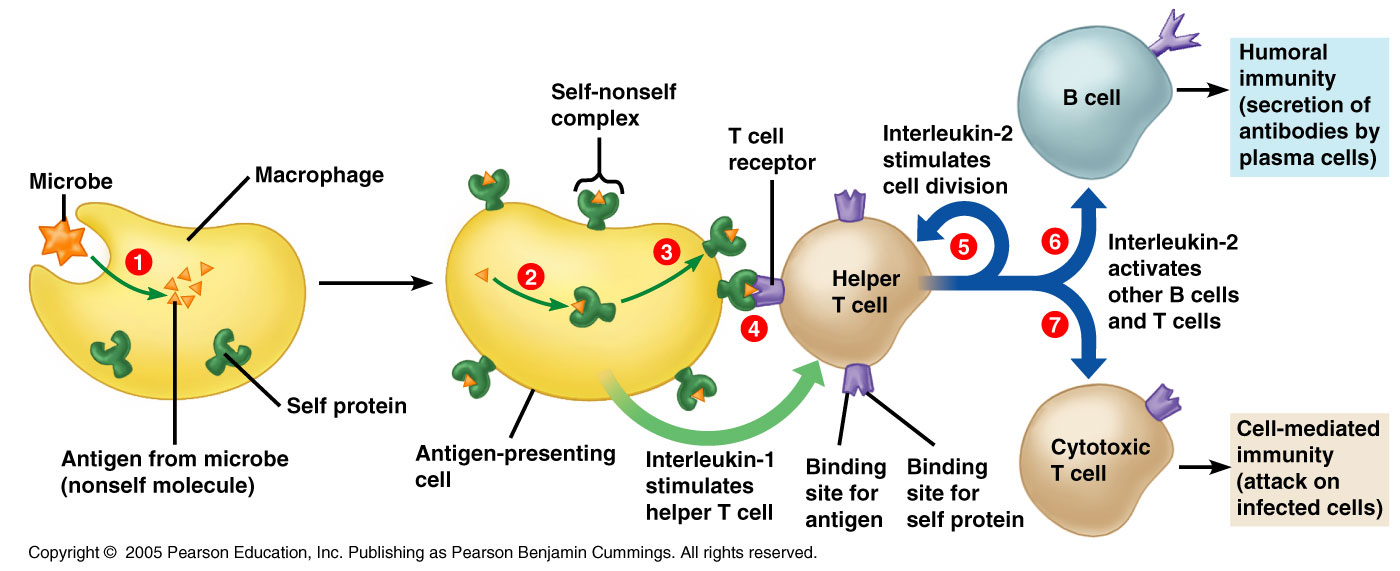
explain the role of B cells, T helper cells (TH 1 and TH 2) and cytotoxic T cells.
-
Recognition phase
- When a body cell is invaded by a bacterium, virus, antigen, etc., the body cell will display on its surface both self markers (antigens) and non-self markers (antigens).
- T cells, which are constantly
patrolling the body, will realize there is a problem.
- Their receptors will recognize the non-self antigens on the surface of the body cell as foreign antigens.
- This indicates that the cell has been invaded.
- Since tissue transplant cells and cancer cells also display these non-self antigens, the T cells will realize there is a problem with these cells also.
-
Response phase
- When T cells recognize
non-self antigens, they go through aclonal selection process
like with B cells.
- The T cell with the receptor for this particular antigen is selected and reproduced in large quantities.
- This allows the immune system to mount a massive attack on the invaded cells.
- Two types of cells are produced:
- Cytotoxic T cells (killer T cells): recognize and destroy non-self cells by puncturing them, causing them to lyse.
- Helper T cells: stimulate the production of cytotoxic T cells and B cells.
- When T cells recognize
non-self antigens, they go through aclonal selection process
like with B cells.
Explain the difference between activity immunity and passive immunity.
Active immunity occurs when the body mounts an immune response to an antigen - effector cells and memory cells are generated.
Passive immunity occurs when a person is given preformed antibodies - no lymphocyte activation, no effector cells, no memory cells.
What is the role of natural killer cells?
- An example of a lymphocyte, a different kind of white blood cell from phagocytes
- Can identify virus infected cells and some tumor cells (cancer cells).
- Kills the cell by attacking the cell membrane, causing the cell to lyse (split open).
How are anti-venoms made?
is created by milking venom from a relevant snake, spider, insect, or fish. The venom is then diluted and injected into a horse, sheep, rabbit, or goat.
Protein deficiency still occurs in many populations throughout the world. Individuals with protein deficiency can be more susceptible to diseases. Explain
- Antibodies are protein--> from amino acids in our diets
- Gets sick much quicker
- Proteins tend to be more expensive: meats
- Mixture of beans and rice are less expensive example of proteins
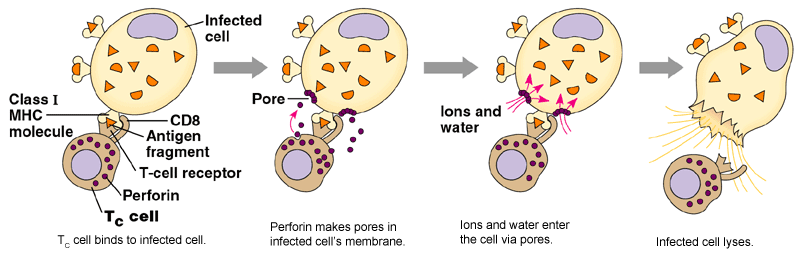
What is the role of activated cytotoxic T cell?
recognize and destroy non-self cells by puncturing them, causing them to lyse
These cells secrete cytotoxin which triggers destruction of the pathogen's DNA or perforin which is a protein that creates holes in the pathogens plasma membrane. The holes cause the pathogen to lyse (rupture).
What is the role of helper T cells in acquired immunity?
These cells secrete interleukin 2 (I-2) which stimulates cell division of T cells and B cells. In other words, these cells recruit even more cells to help fight the pathogen.
Immunologists:
scientists who study the cells and chemicals involved in specific immunity
Cell-mediated immune response
Immune response used by T cells to fight intracellular pathogens and abnormal body cells.
Humoral immune response
The immune response centered around B lymphocytes and antibodies.
Acquired immunity:
The body’s ability to recognize and defend itself against distinct invaders and their products
Is a “smart” system whose “memory’ allows it to respond rapidly to a second encounter with a pathogen
Is acquired over time
Antigens trigger specific immune responses• Various cells, tissues, and organs are part of specific immunity
Includes B and T lymphocytes
Adaptive immunity:
Resistance against pathogens that acts more effectively upon subsequent infections with the same pathogen.
Opsonization
The coating of pathogens by proteins called opsonins, making them more vulnerable to phagocytes
T lymphocytes
(T cell) Lymphocyte that matures in the thymus and acts primarily against endogenous antigens in cell-mediated immune responses.
B Lymphocytes
(B cell) Lymphocyte that arises and matures in the red bone marrow in adults and is found primarily in the spleen, lymph nodes, red bone marrow, and Peyer's patches of the intestines and that secretes antibodies.
Lymphocyte
Type of small agranulocyte, which originates in the red bone marrow and has nuclei that nearly fill the cell.
Antigen
Molecule that triggers a specific immune response.
foreign material
Lymphatic System
is a network of lymph capillaries and larger vessels that empty into the circulatory system
Lymphatic Vessels
tubes that conduct lymph
Lymphoid cells
Develop from stem cells in the red bone marrow
Includes lymphocytes, the smallest of the leukocytes
B lymphocytes(B cells)
T lymphocytes(Tcells)
Lymph
Fluid found in lymphatic vessels that is similar in composition to blood serum and intercellular fluid.
Lymph Nodes
Organs that monitor the composition of lymph
- These nodes essentially “filter” the lymph.
- They are lined with macrophages and lymphocytes, which recognize and destroy pathogens (viruses and bacteria).
- The nodes swell during certain diseases as a result of the accumulation of now-dead lymphocytes, macrophages, and infected cells.
Spleen
Similar function as lymph nodes, except that it filters the blood
Tonsils
Patches of tissue with large numbers of lymphocytes
Mucosa-associated lymphoid disease [MALT]:
made up of peyers patches, the appendix, and the tonsils. It protects passages that are open to the exterior from the never-ending onslaughts of foreign matter entering them
Antibodies:
(immunoglobulin) Proteinaceous antigen-binding molecule secreted by plasma cells.
B Cell receptor [BCR]:
Antibody integral to the cytoplasmic membrane and expressed by B lymphocytes.
Memory B Cells
B lymphocyte that migrates to lymphoid tissues to await a subsequent encounter with antigen previously encountered.
Agglutination
Aggregation (clumping) caused when antibodies bind to two antigens, perhaps hindering the activity of pathogenic microorganisms and increasing the chance that they will be phagocytized.
Neutralization
Antibody function in which the action of a toxin or attachment of a pathogen is blocked.
Cytotoxic T cells:
(Tc cell, CD8 cell) In cell-mediated immune response, type of cell characterized by CD8 cell-surface glycoprotein; secretes perforins and granzymes that destroy infected or abnormal body cells.
Helper T cells
(Th cell, CD4 cell) In cell-mediated immune response, a type of cell characterized by CD4 cell-surface glycoprotein; regulates the activity of B cells and cytotoxic T cells.
CD8:
(cytotoxic T cell, Tc cell) In cell-mediated immune response, type of cell characterized by CD8 cell-surface glycoprotein; secretes perforins and granzymes that destroy infected or abnormal body cells.
Cytokines:
Proteins secreted by many types of cells that regulate adaptive immune responses
Interleukins [ILs]:
Immune system cytokines that signal among leukocytes
Chemokines:
An immune system cytokine that signals leukocytes to rush to the site of inflammation or infection and activate other leukocytes.
Autoantigens:
Antigens on the surface of normal body cells.
Clonal Selection:
In antibody immunity, recognition and activation only of B lymphocytes with BCRs complementary to a specific antigenic determinant.
Major Histocompatibility Complex [MHC]:
A cluster of genes, located on each copy of chromosome 6 in humans, that codes for membrane-bound glycoproteins called major histocompatibility antigens.
Important in determining the compatibility of tissues in successful grafting
MHC class 1:
Found on all cells except red blood cells
MHC class 2
Found on B-cells and antigen-presenting cells
Plasma cells
B cells that are actively fighting against exogenous antigens and secreting antibodies.
Phagolysosome:
APC internalizes the invading pathogen and enzymatically digests it into smaller antigenic fragments which are contained within a phagolysosome
Phagolysosome fuses with a vesicle containing MHCII molecules
CD4:
Distinguishing cytoplasmic membrane protein of helper T cells, which is the initial binding site of HIV.
CD4 cell:
(helper T cell, Th cell) In cell-mediated immune response, a type of cell characterized by CD4 cell-surface glycoprotein; regulates the activity of B cells and cytotoxic T cells.
Dendritic cells
Cells of the epidermis and mucous membranes that devour pathogens.
Anti-venoms:
biological product used in the treatment of venomous bites or stings.
Antivenom is created by milking venom from a relevant snake, spider, insect, or fish. The venom is then diluted and injected into a horse, sheep, rabbit, or goat.
Class-switching:
The process in which a plasma cell changes the type of antibody Fc region (stem) that it synthesizes and secretes.
Adaptive immunity:
attacks particular foreign substances and provides body's 3rd line of defense
Fc Region:
The stem region of an antibody.
IgA:
The antibody class most commonly associated with various body secretions, including tears and milk. IgA pairs with a secretory component to form secretory IgA.
IgG:
The predominant antibody class found in the bloodstream and the primary defender against invading bacteria.
IgM:
The second most common antibody class and the predominant antibody produced first during a primary humoral immune response.
IgD:
A membrane-bound antibody molecule found in some animals as a B cell receptor.
IgE:
Signal antibody molecule that triggers the inflammatory response, particularly in allergic reactions and infections by parasitic worms.
Antigenic determinant:
(epitope) the three- dimensional shape of a region of an antigen that is recognized by the immune system.
The part of the antigen that is recognized
Endogenous antigen:
Antigen produced by microbes that multiply inside the cells of the body.
Tr cell:
(regulatory T cell, suppressor T cell) Thymus-matured lymphocyte that serves to repress adaptive immune responses and prevent autoimmune diseases.
Clonal deletion:
Process by which cells with receptors that responds to autoantigens are selectively killed via apoptosis.
Secretory IgA:
The combination of IgA and a secretory component, found in tears, mucous membrane secretions, and breast milk, where it agglutinates and neutralizes antigens.
Exogenous antigen:
Antigen produced by microorganisms that multiply outside the cells of the body.
T-independent antigens:
Large molecules with repeating subunits that trigger an antibody immune response without the activation of T cells.
Antigen-Binding site:
Site formed by the variable regions of a heavy and light chain of an antibody.
Regulatory T-cell:
(Tr cell, suppressor T cell) Thymus- matured lymphocyte that serves to repress adaptive immune responses and prevent autoimmune diseases.
Artificially acquired passive immunotherapy:
Treatment in which patient receives via injection preformed antibodies in antitoxins or antisera, which can destroy fast-acting and potentially fatal antigens, such as rattlesnake venom.
Artificially acquired active immunity:
occurs when person is given a vaccine
Naturally acquired active immunity
occurs when a person suffers through the symptoms of an infection.
Naturally acquired passive immunity
occurs when a mother’s antibodies enter fetal circulation.
Memory T cell:
Type of T cell that persists in lymphoid tissues for months or years awaiting subsequent contact with an antigenic determinant matching its TCR, at which point it produces cytotoxic T cells.
Th cell:
(helper T cell, CD4 cell) In cell-mediated immune response, a type of cell characterized by CD4 cell-surface glycoprotein; regulates the activity of B cells and cytotoxic T cells.
Apoptosis:
Programmed cell suicide.
Granzyme:
Protein molecule in the cytoplasm of cytotoxic T cells that causes an infected cell to undergo apoptosis.
CD95 pathway:
In cell-mediated cytotoxicity, pathway involving CD95 protein that triggers apoptosis of infected cells.
Epitope:
(antigenic determinant) The three- dimensional shape of a region of an antigen that is recognized by the immune system.
Interferons [IFs]:
Protein molecules that inhibit the spread of viral infections.
Memory response:
The rapid and enhanced immune response to a subsequent encounter with a familiar antigen.
Tc cell:
(cytotoxic T cell, CD8 cell) In cell-mediated immune response, type of cell characterized by CD8 cell-surface glycoprotein; secretes perforins and granzymes that destroy infected or abnormal body cells.
Perforin:
Protein molecule in the cytoplasm of cytotoxic T cells, which forms channels [pores] (perforations) in an infected cell's membrane.
Naturally acquired active immunity:
Type of immunity that occurs when the body responds to exposure to antigens by mounting specific immune responses.
Naturally acquired passive immunity:
Type of immunity that occurs when a fetus, newborn, or child receives antibodies across the placenta or within breast milk.
T-independent antibody immunity:
Adaptive immune response resulting in immunoglobulin production following cross-linking of BCRs on numerous B cells and lacking involvement of helper T cells.
Opsonin:
Antimicrobial protein that enhances phagocytosis.
Primary response:
The slow and limited immune response to a first encounter with an unfamiliar antigen.
Secondary immune response:
Enhanced immune response following a second contact with an antigen.
T-dependent antibody immunity:
Adaptive immune response resulting in immunoglobulin production that requires the action of a specific helper T cell (Th2).
Antigen-presenting cell [APC]:
Dendritic cells, macrophages, and B cells, which process antigens and activate cells of the immune system.
Antibody immune Response [humoral immune response:
The immune response centered around B lymphocytes and antibodies
Antibody-dependent cellular cytotoxity [ADCC]:
Process whereby natural killer lymphocytes (NK cells) lyse cells covered with antibodies.
Growth factor:
Organic chemical, such as a vitamin, required in very small amounts for metabolism. In immunology, an immune system cytokine that stimulates stem cells to divide, ensuring that the body is supplied with sufficient leukocytes of all types.
Synapse:
In immunology, the interface between cells of the immune system that involves cell-to-cell signaling
T-dependent antigens:
Molecules that stimulate an immune response only with the involvement of a helper T cell.
Artificially acquired active immunity:
Type of immunity that occurs when the body receives antigens by injection, as with vaccinations, and mounts a specific immune response
T cell receptor [TCR]:
Antigen receptor generated in the cytoplasmic membrane of T lymphocytes.
Tumor necrosis factor [TNF]:
An immune system cytokine secreted by macrophages and T cells to kill tumor cells and to regulate immune responses and inflammation.
T cell Pathway
- T-cells can either directly destroy the microbes or use chemical secretions to destroy them.
- At the same time, T cells stimulate B cells to divide, forming plasma cells that are able to produce antibodies and memory B cells.
- If the same antigen enters the body later, the memory B cells divide to make more plasma cells and memory cells that can protect against future attacks by the same antigen.
- When the T cells activate (stimulate) the B cells to divide into plasma cells, this is called antibody-mediated immunity.
Cytotoxic T cell pathway
- The cytotoxic T cells are capable of recognizing antigens on the surface of infected body cells.
- The cytotoxic T cells bind to the infected cells and secrete cytotoxins that induce apoptosis (cell suicide) in the infected cell and perforins that cause perforations in the infected cells.
- Both of these mechanisms destroys the pathogen in the infected body cell.
antibody function
Activation of complement
Stimulation of inflammation
Agglutination: so they can’t spread apart and to make it easier for phagocytosis
Neutralization
Opsonization