Instructions for Side by Side Printing
- Print the notecards
- Fold each page in half along the solid vertical line
- Cut out the notecards by cutting along each horizontal dotted line
- Optional: Glue, tape or staple the ends of each notecard together
Health Assessment Exam 1 Chapters 1-6
front 1 What are the core values of medical ethics? Nonmaleficene Beneficence Respect for autonomy Decisional capacity Confidentiality Informed consent Truth telling Justice | back 1
|
front 2 What are proper communication strategies? | back 2
|
front 3 Importance of having an interpreter and how to obtain one? | back 3 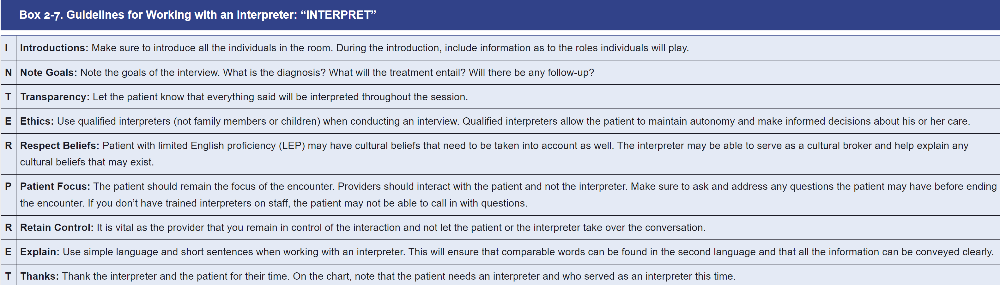
|
front 4 What is objective and subjective history? | back 4
|
front 5 What is in the History of Present Illness? What is in the ROS? What is in the Family and Social History? | back 5 HPI
ROS
Family history
Social History
|
front 6 What does the CAGE Questionnaire mean? | back 6 It is best tool at detecting alcohol dependence. CAGE questions about
Two or more affirmative answers to the CAGE Questionnaire suggest lifetime alcohol abuse and dependence alcohol use disorders (AUDs)
CAGE Questions 1. Have you ever felt you should cut down on your drinking? 2. Have people annoyed you by criticizing your drinking? 3. Have you ever felt bad or guilty about your drinking? 4. Have you ever had a drink first thing in the morning to steady your nerves or to get rid of a hangover (eye-opener)? |
front 7 What is general PE suggested sequence? | back 7
|
front 8 What is proper patient positioning?
| back 8
|
front 9 How do you prioritize patient complains? | back 9
|
front 10 What are the USPSTF screening recs for lung cancer? | back 10
What does the USPSTF recommend?
|
front 11 What is USPSTF screening recs for breast cancer? | back 11 What does the USPSTF recommend?
|
front 12 What is passive immunity | back 12
|
front 13 What is active immunity? | back 13
|
front 14 What is community (herd) immunity? | back 14 Benefits of immunization are not limited to the vaccinated individual but also include promotion of herd immunity for the population at large, including nonimmunized persons and those with waning immunity or who may not have fully responded to prior vaccination |
front 15 Know immunization guidelines | back 15 *** see print paper |
front 16 What are general contraindications for immunizations? | back 16
|
front 17 Is there a link between vaccines and autism? | back 17 No |
front 18 When do you give Tdap, vs Td, vs Dtap? | back 18 Dtap < 7 years old
Tdap > 7 years old
Td is > 7 years
|
front 19 ' What are contraindications of influenza vaccine? | back 19
|