What are the core values of medical ethics?
Nonmaleficene
Beneficence
Respect for autonomy
Decisional capacity
Confidentiality
Informed consent
Truth telling
Justice
-
Nonmaleficence
- (“first, do no harm”) directive that health care professionals should avoid causing harm to patients and minimize the negative effects of treatments.
-
Beneficence
- statement that
clinicians are to act for the patients’ good by
preventing or treating disease.
- statement that
clinicians are to act for the patients’ good by
preventing or treating disease.
-
Respect for autonomy
- commitment to accept the choices patients with decisional capacity make about which treatments to undergo, including to reject treatment.
-
shifts patient -provider relationship from paternalistic
one to a more collaborative
one.
-
Decisional capacity
- ability to make an
autonomous choice that clinicians should respect.
- ability for patients to make there own choice!!
- ability to make an
autonomous choice that clinicians should respect.
-
Confidentiality
- duty to prevent the disclosure of patients’ personal information to parties who are not authorized to learn that information.
- keeping patients info confidential
-
Informed consent
- principle that clinicians must elicit patients’ voluntary and informed authorization to test or treat them for illness or injury.
- Because patients cannot consent to treatment without knowing what they are being treated for, this principle also encompasses the responsibility to inform patients of diagnoses, prognoses, and treatment alternatives.
-
Truth telling
- value that
clinicians should disclose information beyond
that required by informed consent that may be relevant to
patients (e.g., the number of similar procedures a physician has
performed).
- value that
clinicians should disclose information beyond
that required by informed consent that may be relevant to
patients (e.g., the number of similar procedures a physician has
performed).
-
Justice
- treat patients fairly
- all must receive similar treatments/attention
What are proper communication strategies?
-
Ask Me Three
- What is my main
problem?
What do I need to do?
Why is it important for me to do this?
- What is my main
problem?
-
People first language
- identify person before the diagnosis
-
Motivational Interviewing
- 3 core
skills:
• Ask: open ended questions: invite the patient to consider change
• Listen: Listen to the patient and repeat with reflective listening
• Inform: Ask permission to provide information
- 3 core
skills:
-
5
As
- Ask
- Advice
- Assess
- Assist
- Arrange
- Open-ended questions
-
When collaborating: SBAR
- situations
- background
- assessment
- recommendations
-
Moving from Open ended to focus questions
- Start with the most general questions like, “How can I help?” or “What brings you in today?” Then move to still open, but more focused, questions like, “Can you tell me more about what happened when you took the medicine?” Then pose closed questions like, “Did the new medicine cause any problems?”
-
Echoing the patient
- Patient: “The pain got worse and began to spread.” (Pause)
- Response: “Spread?” (Pause)
- Patient: “Yes, it went to my shoulder and down my left arm to the fingers. It was so bad that I thought I was going to die.” (Pause) Response: “Going to die?”
-
Graded response questions
- “How many steps can you climb before you get short of breath?” is better than “Do you get short of breath climbing stairs?”
Importance of having an interpreter and how to obtain one?
- “cultural navigator” who is neutral and trained in both languages and cultures
- Make your questions clear, short, and straightforward.
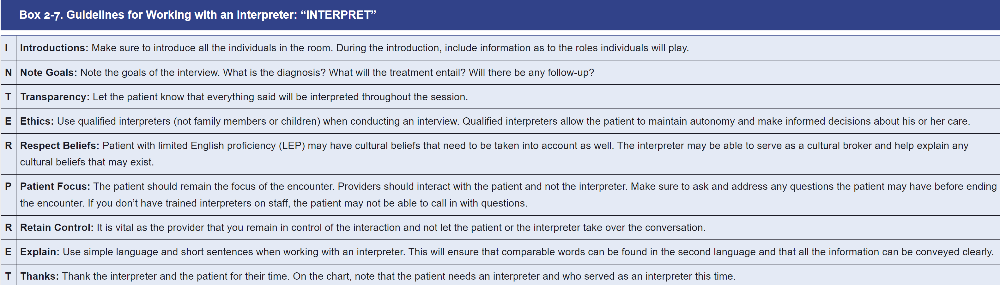
- ** remember interpret
- Telephone interpreting is provided when an interpreter, who is usually based in a remote location, provides interpretation via telephone for two or more individuals who do not speak the same language.
- Face to face interpretation for more
- Serious diagnoses or other bad news
- When the patient is hard-of-hearing
- Family meetings or group discussions
- Interaction requires visual elements
- Complicated or personal medical procedures or news
What is objective and subjective history?
-
Subjective information includes symptoms which are
health concerns that the patient tells you.
- Examples include complaints of a sore throat, headache, or pain.
- It also includes feelings, perceptions, and concerns obtained from the clinical interview.
-
Objective information is the physical examination
findings or signs you detect during the
examination.
- All laboratory and diagnostic testing results are also considered objective information.
- For example, “chest pain” is subjective information while “tenderness on palpation of anterior chest” is an objective one
- Clinical record from the Chief Complaint (CC) through the Review of Systems is considered subjective
- All physical examination, laboratory information and test data are objective information.
What is in the History of Present Illness?
What is in the ROS?
What is in the Family and Social History?
HPI
- HPI is a concise, clear, and chronologic description of the problems prompting the patient’s visit, including the onset of the problem, the setting in which it developed, its manifestations, and any treatments to date.
- The HPI in its most basic form is the story of the patient’s problem
ROS
- Questions may uncover problems or symptoms that you or the patient may have overlooked
- Documents the presence or absence of common symptoms related to each of the major body systems
Family history
- Family History is a record of health information about the patient and his or her immediate relatives.
- It lists the age and health, or age and cause of death, of each immediate relative including parents, grandparents, siblings, children, and grandchildren
Social History
- Purpose is to build rapport with patient
- Social History includes the patient’s Personal History which captures their personality and interests, their coping style, strengths, and concerns.
- Includes their sexual orientation and gender identification (SOGI)
- Place of birth, and personal environmental map
- Occupation and education
- Significant relationships including safety in those relationships
- Home environment including family and household composition
- Important life experiences such as military service, job history, financial situation, and retirement; leisure activities; sexuality, spirituality; and social support systems.
What does the CAGE Questionnaire mean?
It is best tool at detecting alcohol dependence.
CAGE questions about
- Cutting down
- Annoyance when criticized
- Guilty feelings
- Eye openers
Two or more affirmative answers to the CAGE Questionnaire suggest lifetime alcohol abuse and dependence alcohol use disorders (AUDs)
- Scoring 2 out of 4 is highly suggestive of alcohol abuse
CAGE Questions
1. Have you ever felt you should cut down on your drinking?
2. Have people annoyed you by criticizing your drinking?
3. Have you ever felt bad or guilty about your drinking?
4. Have you ever had a drink first thing in the morning to steady your nerves or to get rid of a hangover (eye-opener)?
What is general PE suggested sequence?
- We recommend examining the patient from the patient’s right side, moving to the opposite side or foot of the bed or examining table as necessary
- The key to a thorough and
accurate physical examination is developing a systematic sequence of
examination. Organize your comprehensive or focused examination
around three general goals:
- Maximize the patient’s comfort.
- Avoid unnecessary changes in position.
- Enhance clinical efficiency.
What is proper patient positioning?
- when palpating breast
- cardiovascular assessment- examining JVD vs listening to mitral stenosis?
- abd assessment
- neuro: peripheral vascular assessment
- musc
-
When palpating breast
- The patient position is supine. Ask the patient to lie down. You should stand at the right side of the patient’s bed
-
When examining heart sounds/ JVD
- Elevate the head of the examining table or bed to −30 degrees for the cardiovascular examination, adjusting as necessary to see the jugular venous pulsations.
- Ask the patient to roll partly onto the left side while you listen at the apex for an S3 or mitral stenosis.
- The patient should sit, lean forward, and exhale while you listen for the murmur of aortic regurgitation.
-
Abdomen inspection
- Lower the head of the bed to the flat position. The patient should be supine.
-
Neuro
- When checking peripheral vascular system (femoral pulses/popliteal pulses. Palpate the inguinal lymph nodes, lower extremity edema, discoloration, or ulcers/Palpate for pitting edema, inspect for varicose veins) patient should be SUPINE
-
MUSC
- Checking muscle strength, gait, spine alignment, and movement patient is STANDING
How do you prioritize patient complains?
- ALWAYS RULE OUT THE LIFE-THREATENING CAUSES!!
- One rule of thumb is to always include “the worst-case scenario” in your differential diagnosis and make sure you have ruled out this possibility based on your findings and patient assessment.
- Your goal is to minimize the risk of missing unusual or infrequent conditions such as meningococcal meningitis, bacterial endocarditis, pulmonary embolus, or subdural hematoma that are particularly ominous.
What are the USPSTF screening recs for lung cancer?
What does the USPSTF recommend?
B Grade
- Adults aged 50 to 80 years who have a 20 pack-year smoking
history and currently smoke or have quit
within the past 15 years: - Screen for lung cancer with low-dose computed tomography (CT) every year.
- Stop screening once a person has not smoked for 15 years or has a health problem that limits life expectancy or the ability to have lung surgery
What is USPSTF screening recs for breast cancer?
What does the USPSTF recommend?
- Women aged 40 to 74 years: The USPSTF recommends biennial (every other year) screening mammography.
- Not recommended for women with dense breast
What is passive immunity
- person is given antibodies to a disease rather than producing
them through his or her own immune system
- naturally acquired from the transfer of maternal antibodies via placenta/breastmilk
- passive immunity from antibody-containing blood products/serums (IVIG)
- immediate immunity but does not last long
What is active immunity?
- exposure to a disease organism triggers the immune system to
produce antibodies to that disease
- acquired naturally from disease (chicken pox, hepatitis A)
- Acquired from a vaccine
- active immunity takes several weeks to protect but last a longer than passive
What is community (herd) immunity?
Benefits of immunization are not limited to the vaccinated individual but also include promotion of herd immunity for the population at large, including nonimmunized persons and those with waning immunity or who may not have fully responded to prior vaccination
Know immunization guidelines
*** see print paper
What are general contraindications for immunizations?
-
Vaccination during pregnancy
- Live attenuated viruses should not be administered
- Vaccination of immunocompromised persons
- Should NOT be given live viruses
- Persons with immunocompromised household members should NOT be given varicella, herpes zoster or live flu
- ALLERGY TO streptomycin, neomycin, polymyxin B
- Antibiotic therapy concurrent to vaccine administration only contraindicated in the oral typhoid vaccine
- Lets clear up some things…
- It is OK to give vaccines if a previous local reaction occurred
- It is OK to give vaccines with low-grade fever, mild respiratory, intestinal infections
- Allergy to antibiotics not a contraindications except with allergy to streptomycin, neomycin and polymyxin B
Is there a link between vaccines and autism?
No
When do you give Tdap, vs Td, vs Dtap?
Dtap < 7 years old
- 5-dose series: 2 months, 4 months, 6 months, 15–18 months, and 4–6 years.
Tdap > 7 years old
- Adolescents should receive a single dose of Tdap, preferably at age 11 or 12 years.
- Pregnant people should get a dose of Tdap during every pregnancy, preferably during the early part of the third trimester, to help protect the newborn from pertussis
Td is > 7 years
- usually given as a booster dose every 10 years, or after 5 years in the case of a severe or dirty wound or burn
' What are contraindications of influenza vaccine?
- “flu shot” is an inactivated vaccine containing killed virus
- DO NOT GIVE IF:
- < 6 months old
- History of severe allergic reaction (e.g., anaphylaxis) to any component of the vaccine (other than egg) or to a previous dose of any influenza vaccine (i.e, any egg-based IIV, ccIIV, RIV, or LAIV of any valency)
- At the same time as aspirin or salicylate-containing therapy in children and adolescents
- Children aged 2 through 4 years who have received a diagnosis of asthma or whose parents or wheezing episode has occurred during the preceding 12 months
- Children and adults who are immunocompromised due to any cause, including but not limited to medications, congenital or acquired immunodeficiency states, HIV infection, anatomic asplenia, or functional asplenia (e.g., due to sickle-cell anemia)
- Close contacts and caregivers of severely immunosuppressed persons who require a protected environment
- Pregnancy
- Persons with active communication between the CSF and the oropharynx, nasopharynx, nose, or ear or any other cranial CSF leak
- Persons with cochlear implants (due to potential for CSF leak, which might exist for some period of time after implantation. Providers might consider consultation with a specialist concerning risk of persistent CSF leak if an age- appropriate inactivated or recombinant vaccine cannot be used)
- Taking influenza antiviral medication within the previous 48 hours for oseltamivir and zanamivir, 5 days for peramivir, and 17 days