| back 1 ➢Regulates the function of many different types of cells & organs
It Affects:
➢Energy metabolism
➢Growth and development
➢Muscle distribution
➢Sexual development
➢Fluid and electrolyte balance
➢Inflammatory/immune responses |
front 2
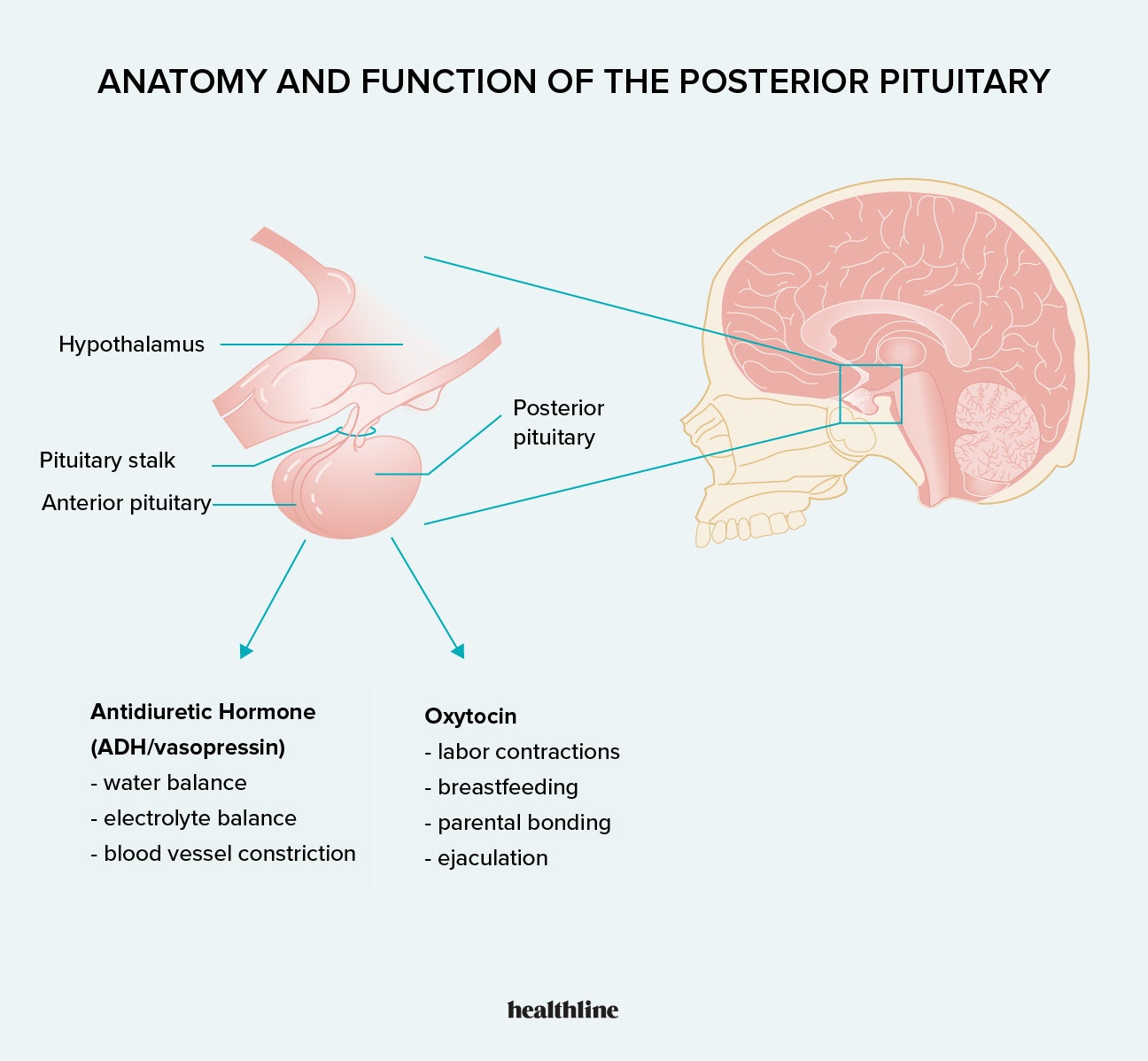
Disorder of Posterior Pituitary
Syndrome of Antidiuretic Hormone Secretion (SIADH)
What is it?
What is most common cause, other causes?
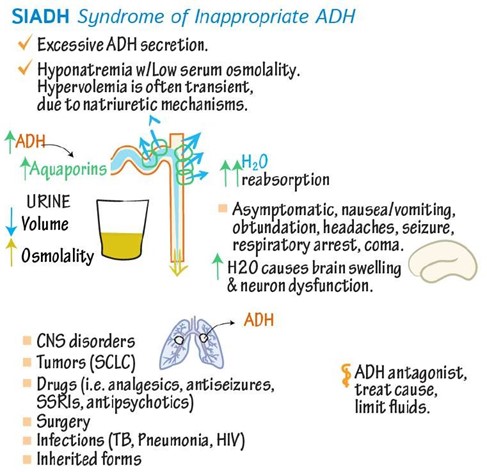
What are diagnosis results? | back 2 - Elevated levels of antidiuretic hormone (ADH)
- Water
retention: the action of ADH on renal collecting ducts increases
their permeability to water, thus increasing water reabsorption by
the kidneys
Causes
-
SIADH secretion is associated with certain forms of cancer,
apparently because of ECTOPIC SECRETION
OF ADH FROM TUMOR cells is the most
common cause
- Also common after surgery
(5-7 days @ risk, likely related to fluid and volume changes
following surgery, the amount and type of intravenous fluids
given, and the use of narcotic analgesics) and some cancers
(small cell carcinoma)
Diagnosis Results
- For diagnosis: NORMAL renal,
adrenal, and thyroid function must exist
|
front 3 Syndrome of Antidiuretic Hormone Secretion (SIADH) Clinical Manifestations | back 3
*Retaining water
- Hypervolemia
- Weight gain
- Hyponatremia:
sodium <135 mEq/L bc dilutional
- Hypoosmolality:
<280 mOsm/kg
- Urine hyperosmolality: higher than serum
osmolality
- Serum sodium levels below 110–115 mEq/L: can cause
severe and sometimes irreversible neurologic damage
|
| back 4 - Correction of underlying causal problems
-
Most
important: fluid restriction between 800 and
1000 mL/day
- Emergency correction of severe hyponatremia by the
administration of hypertonic saline
- Vaptans (vasopressin
receptor antagonists)
- Resistant or chronic SIADH:
- demeclocycline (tetracycline antibiotic:
works on collecting tubules to not hold onto
water)
|
front 5
Disorder of Posterior Pituitary
Diabetes Insipidus
What is it?
What are 3 different types? | back 5
- Insufficiency of ADH
- Polyuria and
polydipsia
- Partial or total inability to concentrate the
urine
-
3 Types:
-
Neurogenic or Central
- Insufficient amounts of ADH (any organic lesion of the
hypothalamus, pituitary stalk, or posterior pituitary
interferes with ADH synthesis, transport, or
release)
-
Nephrogenic
- Insensitivity of the
renal collecting tubules to ADH
-
Dipsogenic
- Excessive fluid
intake, lowering plasma osmolarity to the point that it falls
below the threshold for ADH secretion
|
front 6
Disorder of Posterior Pituitary
Diabetes Insipidus Characteristics
plasma osmolality?
urine output? | back 6 - Is characterized by the inability of the kidney to increase
permeability to water
-
diabetes insipidus have a partial to total inability to
concentrate urine
-
Insufficient ADH activity causes excretion of
large volumes of dilute urine, leading to
increased plasma osmolality.
- Characteristics
-
Increase in plasma osmolality : >300
mOsm/kg, depending on adequate water intake
-
Urine
output: 8–12 L/day for DI patients
*Osmolality indicates the concentration of all the particles
dissolved in body fluid. |
front 7
Disorder of Posterior Pituitary
Diabetes Insipidus S/S? | back 7
- Polyuria, Nocturia, Diuresis
- Continual
thirst
- Hypernatremia (bc losing fluid)
- Low
urine-specific gravity: <1.010
- Low urine osmolality
(<200 mOsm/kg)
|
front 8
Disorder of Posterior Pituitary
Diabetes Insipidus Treatment? | back 8 -
Treatment
-
Neurogenic:
- administration of the
synthetic vasopressin analog desmopressin acetate
(DDAVP)
-
Nephrogenic:
- treatment of any
reversible underlying disorders or discontinuation of problem
medications
- Correction of associated electrolyte
disorders
- Administration of thiazide
diuretics (thiazide diuretics may
improve renal tubular salt and water retention in
individuals with
moderate nephrogenic
DI) -
Dipsogenic: effective management of water
ingestion
|
front 9
Adrenal Glands Function
What hormones does it produce, in the cortex and medulla? | back 9 -
Medulla: part of the sympathetic nervous system
- produces epinephrine/norepinephrine
-
Cortex: secretes 3 types of hormones
- Glucocorticoids
(i.e.. Cortisol)
- Regulates response to stress and controls the
inflammatory response
- Mineralocorticoids
(i.e.. Aldosterone)
- Regulates sodium levels and water balance
- Adrenal
androgens
- Regulates pubertal growth of body hair
|
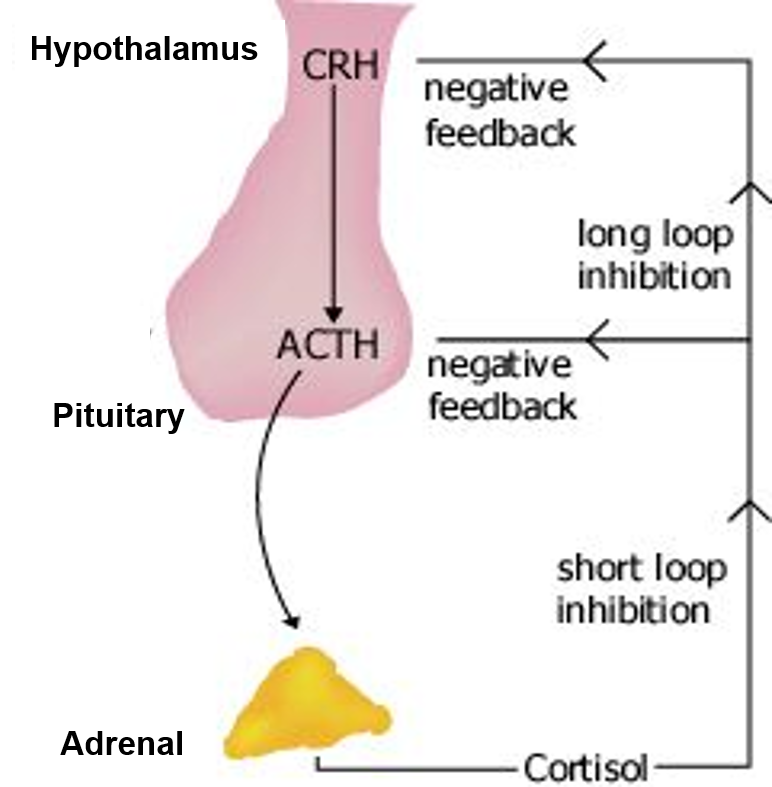
front 10
Alterations in Adrenal Function
Cushing Syndrome/Disease (adrenal cortex)
What is it? What hormone is elevated?
What are causes? | back 10 - Elevated levels of cortisol
Causes
- Pituitary dysfunction in which ACTH is excessively produced
due to pituitary tumor (Cushing Disease)
- excess
ACTH stimulates excess production of cortisol and there is loss
of feedback control of ACTH secretion
- Adrenal tumor
- A tumor somewhere else in body making
ACTH (i.e.. small cell carcinoma lung cancer)
- Long
term prescription glucocorticoid use (Cushing Syndrome)
|
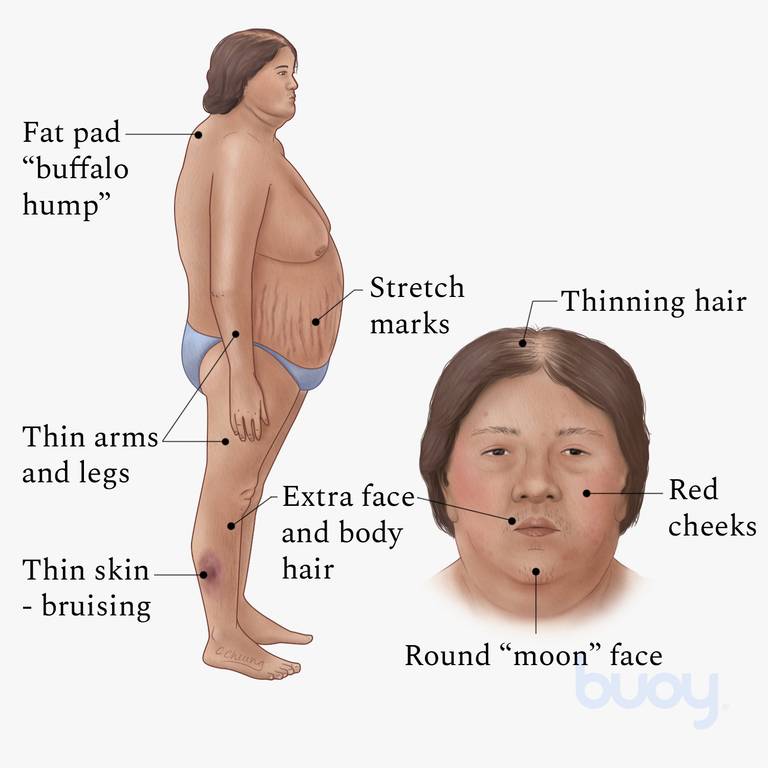
front 11
Alterations in Adrenal Function
Cushing Syndrome/Disease S/S? | back 11 - Weight gain is the most common feature
- Transient
weight gain from sodium and water retention
- because of the
mineralocorticoid effects of cortisol
- Accumulation of adipose tissue in the trunk, facial, and
Cervical areas (NECK)
- Moon face
- Buffalo hump
- Trucal central obesity
- Polyuria, Nocturia, Diuresis
- caused from glucose
intolerance & cortisol-induced insulin resistance and
increased gluconeogenesis and glycogen storage by the
liver
|
front 12
Alterations in Adrenal Function
Cushing Syndrome/Disease Treatment | back 12 -
Treatment
- surgery- first
level treatment to get rid of tumor
- medication
- radiation
|
front 13
Alterations in Adrenal Function
Addison Disease (adrenal cortex)
What is it?
Causes? | back 13 - Primary adrenal cortical insufficiency
-
develops because of a primary inability of the adrenals to
produce and secrete the adrenocortical hormones
-
Causes
- Auto-immune destruction of adrenal cortex
- Infections: Fungal infection
- Bilateral adrenal
hemorrhage
- Drugs (i.e.. ketoconazole) prolong use of
fungal drug
|
front 14
Alterations in Adrenal Function
Addison Disease (adrenal cortex) S/S? | back 14 - Early Features: dehydration, weakness, and fatigue
- Hyperpigmentation (bronze skin)
- Hypoglycemia
- Postural hypotension
- Weight loss
|
front 15
Alterations in Adrenal Function
Addison Disease (adrenal cortex) | back 15 -
Treatment
- Lifetime glucocorticoid and mineralocorticoid (florinef)
replacement therapy
|
front 16
Alterations in Adrenal Function
Pheochromocytoma (adrenal medulla)
What is it?
S/S?
Treatment? | back 16 - Caused by tumors derived from the chromaffin cells of the
adrenal medulla
- Tumors secrete catecholamines
-
Clinical
manifestations
- Hypertension
- Diaphoresis
- Tachycardia, palpitations
- Severe
headache
-
Treatment
- Alpha and beta
blockers for hypertension
- Laparoscopic surgical excision
of the tumor, radiation, or chemotherapy
|
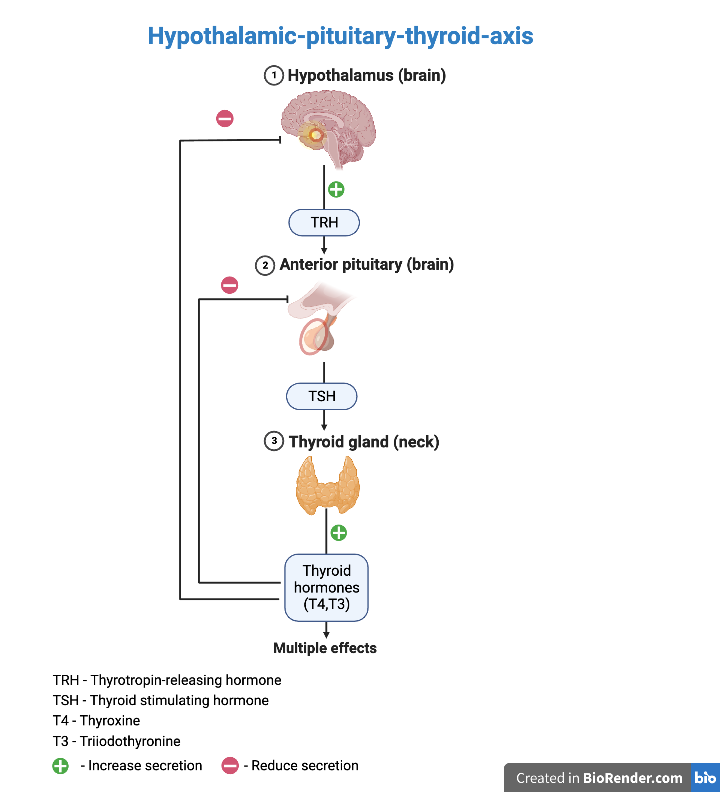
front 17 Thyroid Hormones and Function & Negative Feedback Loop | back 17
Thyrotropin
releasing hormone (TRH)
- secreted by the hypothalamus, and acts on the anterior
pituitary to stimulate release of thyroid stimulating hormone
(TSH).
- The release of TRH is inhibited in the presence of
high levels of circulating T3 and T4.
Thyroid
stimulating hormone (TSH)
- secreted by the anterior pituitary, in response to the
stimulating effect of TRH.
- TSH acts on the thyroid gland to
stimulate release of T3 and T4.
- The release of TSH is
inhibited in the presence of high levels of circulating T3 and
T4.
Thyroxine (T4)
- produced by the thyroid gland in response to the
stimulating effect of TSH.
- Thyroxine is transported in
plasma in either its free form or bound to protein.
- Thyroxine is converted to T3 and reverse T3 (rT3) in both the
circulation and in tissues.
Triiodothyronine (T3)
- directly secreted by the thyroid and converted from T4
Reverse
triiodothyronine (rT3)
- is an inactive form of T3 that is secreted in stress
states
|
front 18
Alterations in Thyroid Function
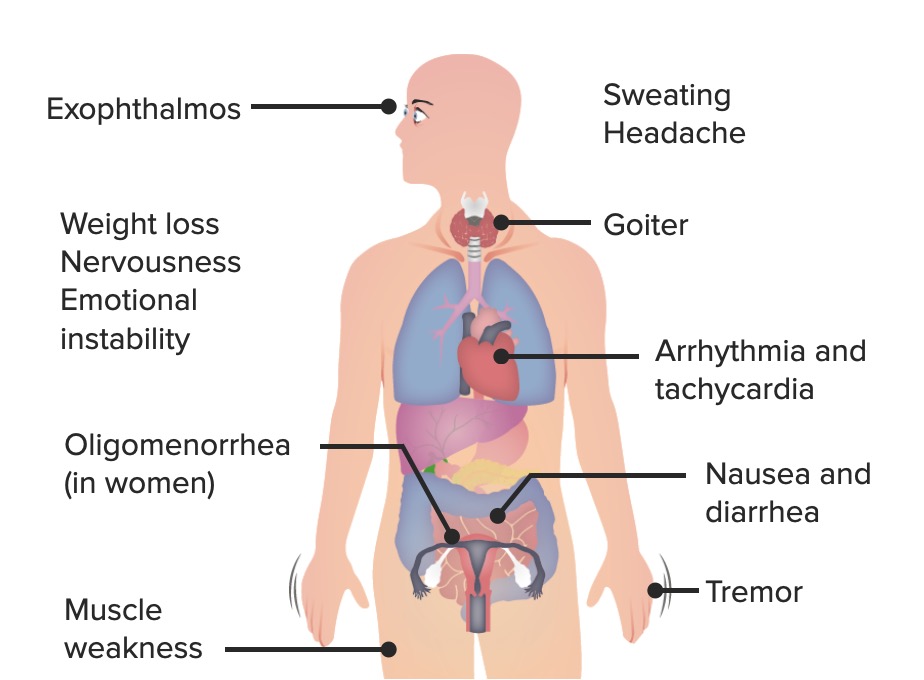
Hyperthyroidism: Thyrotoxicosis | back 18 - Is a condition that results from any cause of increased level
of thyroid hormone
- Excess amounts of thyroid hormone are
secreted from the thyroid gland
-
Clinical
manifestations
- Increased metabolic rate
with heat intolerance
- Increased sympathetic nervous
system
-
Enlargement of the thyroid gland
(goiter)
-
Treatment
- Antithyroid drugs: Methimazole or propylthiouracil
(PTU)
- Radioactive iodine therapy: absorbed only by
thyroid tissue, causing death of cells
- Surgery
|
front 19
Alterations in Thyroid Function
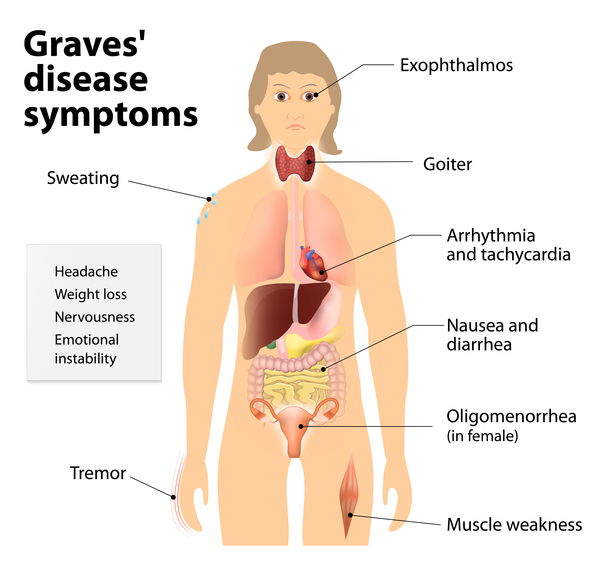
Hyperthyroidism: Graves Disease | back 19
Type II hypersensitivity: infiltration of lymphocytes
and thyroid autoantibodies attack TSH receptor and override normal
negative feedback mechanisms
-
Clinical
manifestations
- Exophthalmos:
increased secretion of hyaluronic acid, orbital fat
accumulation, inflammation, and edema of the orbital
contents
- Diplopia: double
vision
- Ophthalmopathy:
enlargement of the ocular muscles,autoimmune
inflammatory disorder of the orbit and periorbital
tissues,
- Pretibial myxedema
(Graves dermopathy): leg swelling; subcutaneous swelling on
the anterior portions of the legs and by indurated
-
Treatment
- Antithyroid drugs,
radioactive iodine, or surgery
- Does not reverse
infiltrative ophthalmopathy or pretibial myxedema
|
front 20
Alterations in Thyroid Function
Hyperthyroidism: Thyroid Storm | back 20 - Rare but life threatening within 48 hours if not treated
- Increased action of thyroxine (T4) and triiodothyronine
(T3)
-
Clinical
manifestations
- Hyperthermia
-
tachycardia, especially atrial tachydysrhythmias;
high-output heart failure
- agitation
or delirium
- nausea, vomiting, or diarrhea
-
Treatment I.S.
A.B.C.
- Iodine (saturated solution of
potassium iodide [SSKI])
- iodine blocks the
release of T4 and T3 from the gland within
hours
- Supportive care
- Antithyroid Drugs: Propyl-thio-uracil or
methimazole
- blocks thyroid hormone
synthesis
- Beta-blockers to control
cardiovascular symptoms,
- Corticosteroids - reduces
the conversion of T4 to T3
|
front 21
Alterations in Thyroid Function
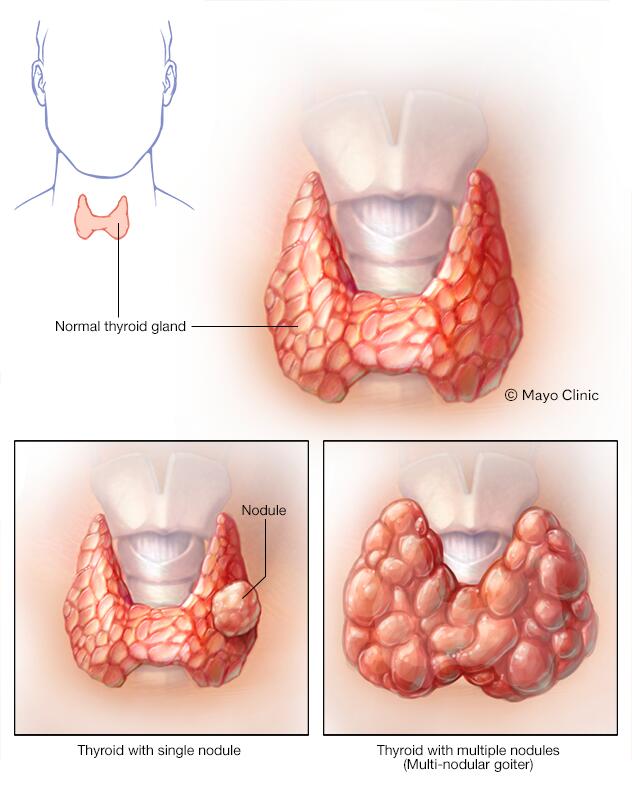
Hyperthyroidism: Nodular Thyroid Disease | back 21 - Hyperthyroidism resulting from nodular thyroid
disease
- Toxic multinodular goiter:
several
hyperfunctioning nodules secrete thyroid hormone
-
Solitary toxic
adenoma: only one
nodule becomes hyperfunctioning
-
Clinical
manifestations
- Are the same as
hyperthyroidism but occur
slowly
-
Exophthalmos and pretibial myxedema DO NOT
occur
-
Treatment
- Must rule out cancer
- Radioactive iodine, surgery, or antithyroid drugs are
administered
|
front 22
Alterations in Thyroid Function
Primary Hypothyroidism
What is it?
What are different types? | back 22 - Deficient production of thyroid hormone by the thyroid
gland
- Hypothyroidism results from deficient
production of TH by the thyroid gland. Hypothyroidism is the
most common disorder of thyroid
function
Types
-
Iodine deficiency
(endemic goiter): most common worldwide
- Autoimmune
thyroiditis (Hashimoto disease): most common
hypothyroidism in the United States
-
Postpartum
thyroiditis- check post partum women for thyroid levels
|
front 23 Congenital hypothyroidism
What is it?
What can it cause if not treated?
How can it be prevented?
Treatment? | back 23 - Present at birth: Due to either: ➢Congenital lack of
thyroid gland Or ➢Abnormal making of
thyroid hormone
- Thyroid hormone deficiency present at
birth
-
Consequences if left untreated
- If not treated, Cretinism develops
(stunted physical and mental growth due to untreated
congenital deficiency of thyroid hormones)
-
Prevention
- Neonatal screening
to reduce incidents
Treatment
|
front 24 - Thyroid carcinoma
- What is the most common cause?
- Characteristics?
| back 24 - Thyroid carcinoma
-
Most
common endocrine malignancy from ionizing
radiation
-
Characteristics
- Changes in voice and swallowing and
difficulty in breathing, related to a tumor growth impinging the
trachea or esophagus
- Most individuals with thyroid
carcinoma have normal T3 and T4 levels
Thyroid cancer typically is discovered as a small thyroid nodule
or as a metastatic tumor
diagnostic test: fine needle biopsy of thyroid |
| back 25 - Clinical manifestations "3Ls
1D"
- Low basal metabolic rate
- Low basal body temp: cold intolerance
- Low energy:
tiredness/lethargy
- Possible Diastolic hypertension
|
front 26 Hypothyroidism
- Myxedema What is it?
- What is myxedema coma?
s/s?
| back 26 -
What is
it
- sign of severe or
long-standing hypothyroidism
-
Causes
- Precipitating events
include infections, discontinuation of thyroid supplements,
overuse of narcotics or sedatives, or a consequence of an
acute illness in individuals who have
hypothyroidism
S/S
- Myxedema
- Nonpitting, boggy edema, especially
around the eyes, hands, and feet; thickening of the tongue
- Medical emergency, diminished level of
consciousness
- hypothermia without shivering
- hypoventilation
- hypotension
- hypoglycemia
- lactic acidosis and coma
|
| back 27
- Levothyroxine (synthetic hormone)
- Myxedema coma
- Thyroid hormone,
combined with circulatory and ventilatory support
- Management of hyponatremia and hypothermia
|
front 28
* EXTRA Function of Parathyroid Hormone | back 28 -
Release of calcium by bones into the
bloodstream.
- Absorption of calcium from food by the
intestines.
- Conservation of calcium by the kidneys
|
front 29
Alterations in Parathyroid Function
Hyperparathyroidism What is it? Two different causes? | back 29
Causes
-
Primary
hyperparathyroidism
- Excess secretion of PTH from
one or more parathyroid glands and hypercalcemia
occurs
- 80%–85% caused by parathyroid adenomas
-
Secondary
hyperparathyroidism
- Increase in PTH, secondary to
a chronic disease
- Chronic renal failure
- Dietary
deficiency of vitamin D, calcium
-
Hypercalcemia does
not occur
|
front 30
Alterations in Parathyroid Function
Hyperparathyroidism S/S of primary & secondary & Treatment | back 30 -
Clinical
manifestations
-
Primary:
- Most asymptomatic
- Hypercalcemia and hypophosphatemia
- possible kidney
stones from hypercalciuria
- alkaline urine
- pathologic fractures bc inc CA leeched out of the bones
into the blood
-
Secondary:
- low
serum calcium but elevated PTH
-
Treatment
- Surgery,
bisphosphonates, corticosteroids, and calcimimetics
|
front 31
Alterations in Parathyroid Function
Hypoparathyroidism What is it? Causes? | back 31 - Abnormally low PTH levels
- Depressed serum calcium
level
- Increased serum phosphate level
- Usual
causes:
- parathyroid damage in thyroid surgery
- autoimmunity
- genetic mechanisms
|
front 32 Alterations in Parathyroid Function
Hypoparathyroidism S/S & Treatment | back 32 -
Clinical
manifestations * S/S of low Ca
- Hypocalcemia
- Muscle spasms/hyperreflexia
- Convulsions
- Laryngeal spasms
- Chvostek and
Trousseau signs
- Phosphate retention
-
Treatment
- Calcium and vitamin
D
- Phosphate binders, if needed
|