Endocrine Function
➢Regulates the function of many different types of cells & organs
It Affects:
➢Energy metabolism
➢Growth and development
➢Muscle distribution
➢Sexual development
➢Fluid and electrolyte balance
➢Inflammatory/immune responses
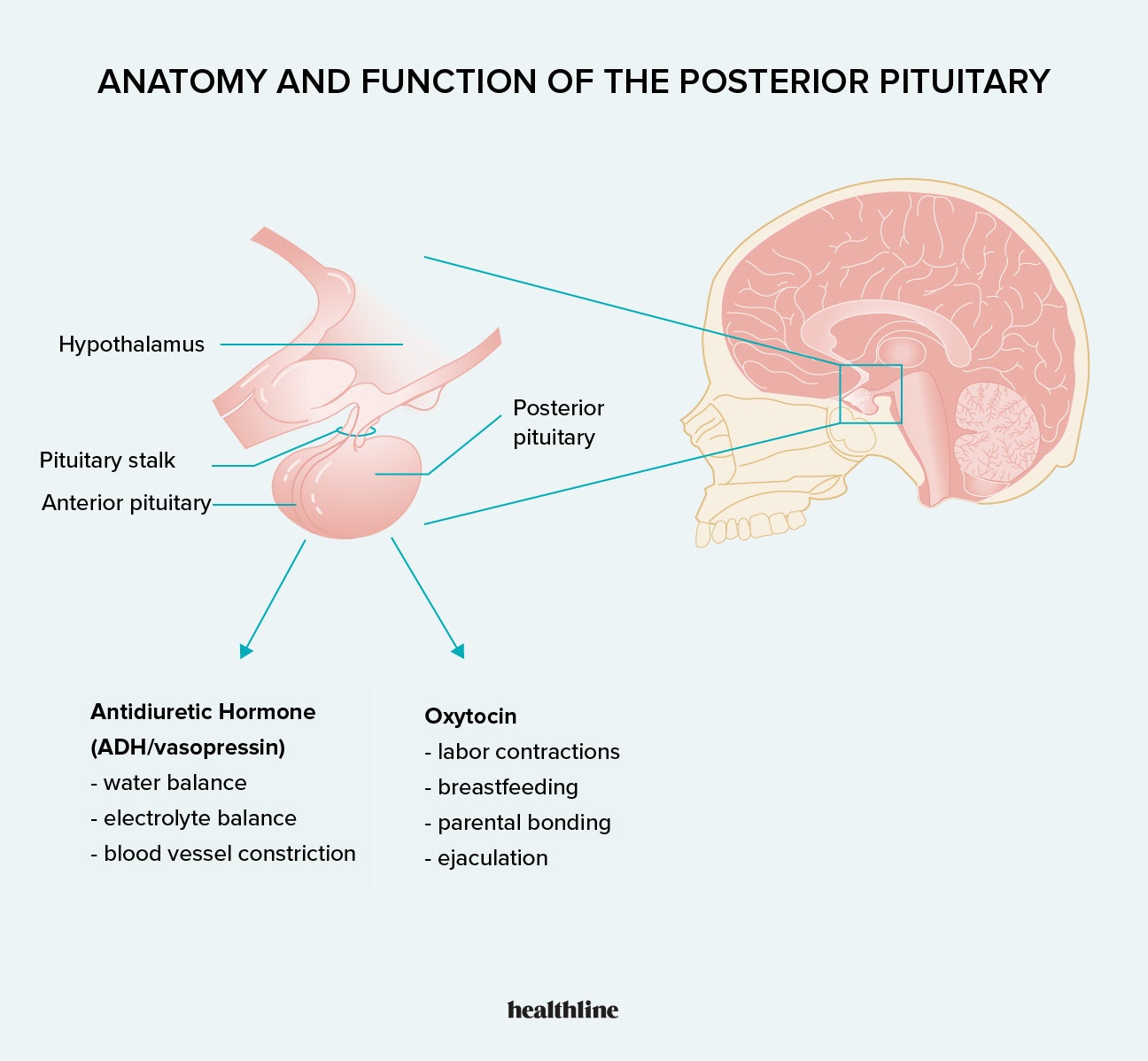
Disorder of Posterior Pituitary
Syndrome of Antidiuretic Hormone Secretion (SIADH)
What is it?
What is most common cause, other causes?
What are diagnosis results?

- Elevated levels of antidiuretic hormone (ADH)
- Water retention: the action of ADH on renal collecting ducts increases their permeability to water, thus increasing water reabsorption by the kidneys
Causes
- SIADH secretion is associated with certain forms of cancer, apparently because of ECTOPIC SECRETION OF ADH FROM TUMOR cells is the most common cause
- Also common after surgery (5-7 days @ risk, likely related to fluid and volume changes following surgery, the amount and type of intravenous fluids given, and the use of narcotic analgesics) and some cancers (small cell carcinoma)
Diagnosis Results
- For diagnosis: NORMAL renal, adrenal, and thyroid function must exist
Syndrome of Antidiuretic Hormone Secretion (SIADH) Clinical Manifestations

*Retaining water
- Hypervolemia
- Weight gain
- Hyponatremia: sodium <135 mEq/L bc dilutional
- Hypoosmolality: <280 mOsm/kg
- Urine hyperosmolality: higher than serum osmolality
- Serum sodium levels below 110–115 mEq/L: can cause severe and sometimes irreversible neurologic damage
SIADH Treatment
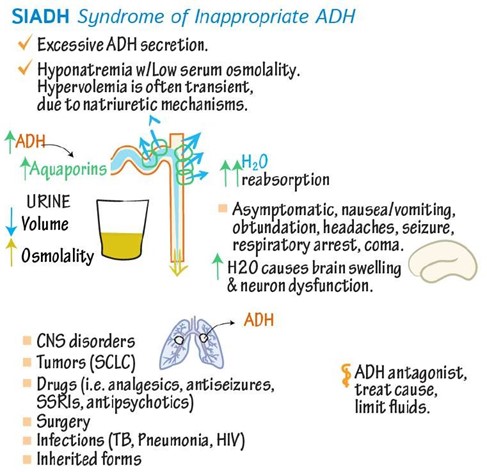
- Correction of underlying causal problems
-
Most
important: fluid restriction between 800 and
1000 mL/day
- Emergency correction of severe hyponatremia by the administration of hypertonic saline
- Vaptans (vasopressin receptor antagonists)
- Resistant or chronic SIADH:
- demeclocycline (tetracycline antibiotic: works on collecting tubules to not hold onto water)
Disorder of Posterior Pituitary
Diabetes Insipidus
What is it?
What are 3 different types?
- Diabetes insipidus
- Insufficiency of ADH
- Polyuria and polydipsia
- Partial or total inability to concentrate the urine
- 3 Types:
- Neurogenic or Central
- Insufficient amounts of ADH (any organic lesion of the hypothalamus, pituitary stalk, or posterior pituitary interferes with ADH synthesis, transport, or release)
- Nephrogenic
- Insensitivity of the renal collecting tubules to ADH
- Dipsogenic
- Excessive fluid intake, lowering plasma osmolarity to the point that it falls below the threshold for ADH secretion
Disorder of Posterior Pituitary
Diabetes Insipidus Characteristics
plasma osmolality?
urine output?
- Is characterized by the inability of the kidney to increase permeability to water
- diabetes insipidus have a partial to total inability to concentrate urine
- Insufficient ADH activity causes excretion of large volumes of dilute urine, leading to increased plasma osmolality.
- Characteristics
- Increase in plasma osmolality : >300 mOsm/kg, depending on adequate water intake
-
Urine
output: 8–12 L/day for DI patients
- normal output: 1–2 L/day
*Osmolality indicates the concentration of all the particles dissolved in body fluid.
Disorder of Posterior Pituitary
Diabetes Insipidus S/S?
- Clinical manifestations
- Polyuria, Nocturia, Diuresis
- Continual thirst
- Hypernatremia (bc losing fluid)
- Low urine-specific gravity: <1.010
- Low urine osmolality (<200 mOsm/kg)
Disorder of Posterior Pituitary
Diabetes Insipidus Treatment?
- Treatment
-
Neurogenic:
- administration of the synthetic vasopressin analog desmopressin acetate (DDAVP)
-
Nephrogenic:
- treatment of any reversible underlying disorders or discontinuation of problem medications
- Correction of associated electrolyte disorders
- Administration of thiazide
diuretics (thiazide diuretics may
improve renal tubular salt and water retention in individuals with
moderate nephrogenic DI)
- Dipsogenic: effective management of water ingestion

Adrenal Glands Function
What hormones does it produce, in the cortex and medulla?
-
Medulla: part of the sympathetic nervous system
- produces epinephrine/norepinephrine
-
Cortex: secretes 3 types of hormones
- Glucocorticoids
(i.e.. Cortisol)
- Regulates response to stress and controls the inflammatory response
- Mineralocorticoids
(i.e.. Aldosterone)
- Regulates sodium levels and water balance
- Adrenal
androgens
- Regulates pubertal growth of body hair
- Glucocorticoids
(i.e.. Cortisol)
Alterations in Adrenal Function
Cushing Syndrome/Disease (adrenal cortex)
What is it? What hormone is elevated?
What are causes?
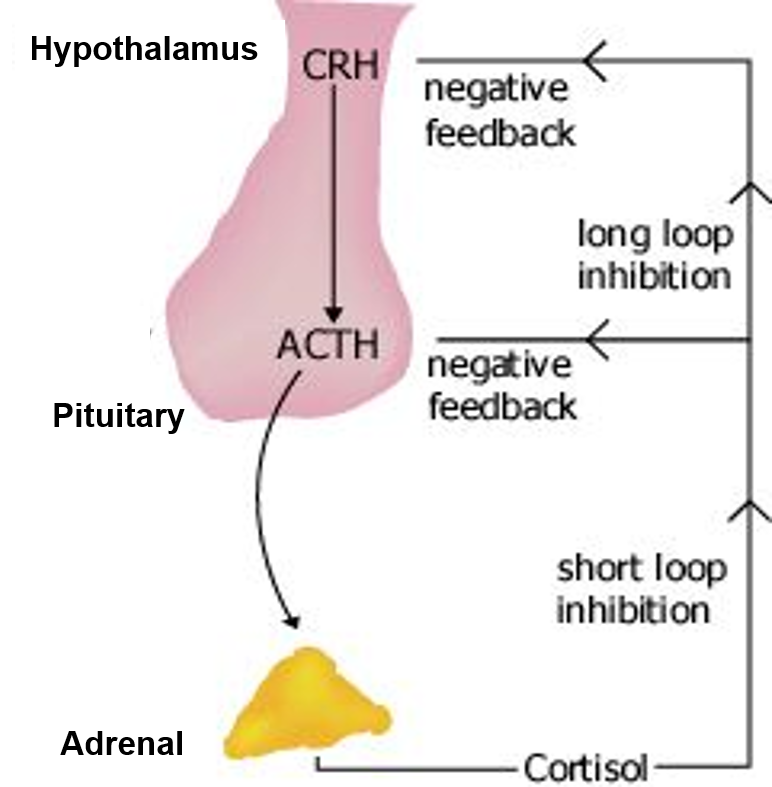
- Elevated levels of cortisol
Causes
- Pituitary dysfunction in which ACTH is excessively produced
due to pituitary tumor (Cushing Disease)
- excess ACTH stimulates excess production of cortisol and there is loss of feedback control of ACTH secretion
- Adrenal tumor
- A tumor somewhere else in body making ACTH (i.e.. small cell carcinoma lung cancer)
- Long term prescription glucocorticoid use (Cushing Syndrome)
Alterations in Adrenal Function
Cushing Syndrome/Disease S/S?
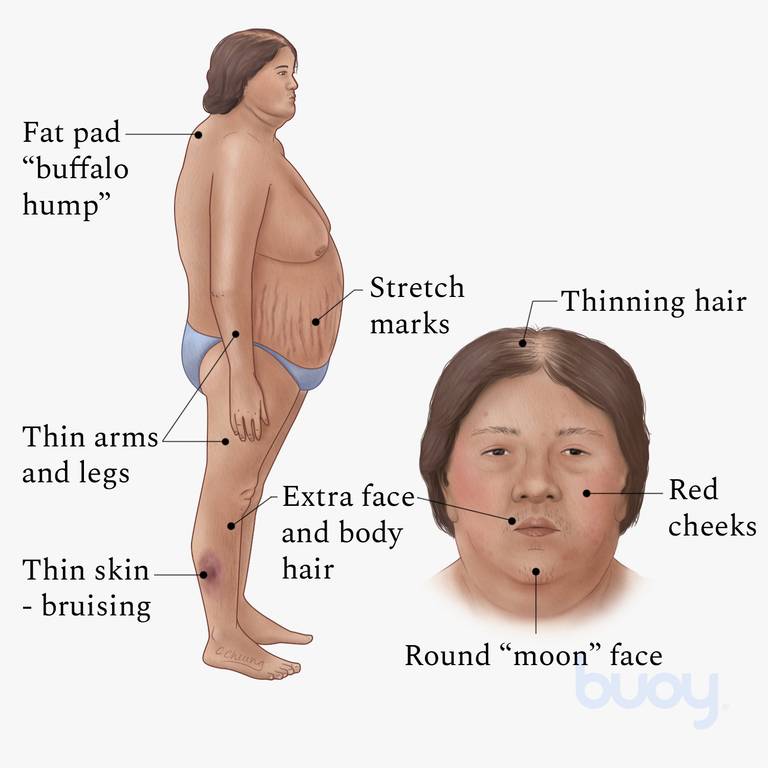
- Weight gain is the most common feature
- Transient
weight gain from sodium and water retention
- because of the mineralocorticoid effects of cortisol
- Accumulation of adipose tissue in the trunk, facial, and
Cervical areas (NECK)
- Moon face
- Buffalo hump
- Trucal central obesity
- Polyuria, Nocturia, Diuresis
- caused from glucose intolerance & cortisol-induced insulin resistance and increased gluconeogenesis and glycogen storage by the liver
Alterations in Adrenal Function
Cushing Syndrome/Disease Treatment
- Treatment
- surgery- first level treatment to get rid of tumor
- medication
- radiation

Alterations in Adrenal Function
Addison Disease (adrenal cortex)
What is it?
Causes?
- Primary adrenal cortical insufficiency
- develops because of a primary inability of the adrenals to produce and secrete the adrenocortical hormones
-
Causes
- Auto-immune destruction of adrenal cortex
- Infections: Fungal infection
- Bilateral adrenal hemorrhage
- Drugs (i.e.. ketoconazole) prolong use of fungal drug
Alterations in Adrenal Function
Addison Disease (adrenal cortex) S/S?
- Early Features: dehydration, weakness, and fatigue
- Hyperpigmentation (bronze skin)
- Hypoglycemia
- Postural hypotension
- Weight loss
Alterations in Adrenal Function
Addison Disease (adrenal cortex)
- Treatment
- Lifetime glucocorticoid and mineralocorticoid (florinef) replacement therapy
Alterations in Adrenal Function
Pheochromocytoma (adrenal medulla)
What is it?
S/S?
Treatment?

- Caused by tumors derived from the chromaffin cells of the adrenal medulla
- Tumors secrete catecholamines
- Clinical manifestations
- Hypertension
- Diaphoresis
- Tachycardia, palpitations
- Severe headache
- Treatment
- Alpha and beta blockers for hypertension
- Laparoscopic surgical excision of the tumor, radiation, or chemotherapy
Thyroid Hormones and Function & Negative Feedback Loop
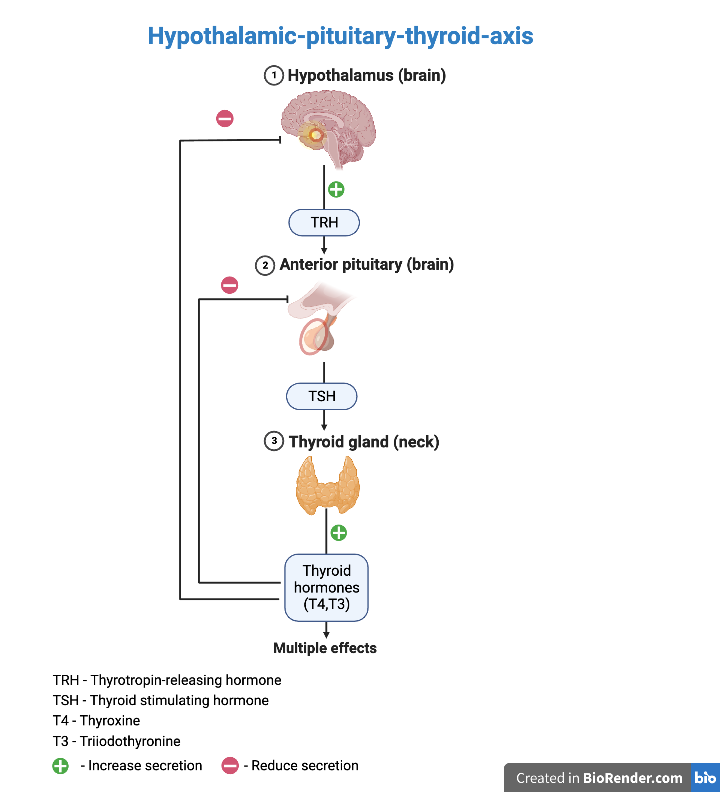
Thyrotropin releasing hormone (TRH)
- secreted by the hypothalamus, and acts on the anterior pituitary to stimulate release of thyroid stimulating hormone (TSH).
- The release of TRH is inhibited in the presence of high levels of circulating T3 and T4.
Thyroid stimulating hormone (TSH)
- secreted by the anterior pituitary, in response to the stimulating effect of TRH.
- TSH acts on the thyroid gland to stimulate release of T3 and T4.
- The release of TSH is inhibited in the presence of high levels of circulating T3 and T4.
Thyroxine (T4)
- produced by the thyroid gland in response to the stimulating effect of TSH.
- Thyroxine is transported in plasma in either its free form or bound to protein.
- Thyroxine is converted to T3 and reverse T3 (rT3) in both the circulation and in tissues.
Triiodothyronine (T3)
- directly secreted by the thyroid and converted from T4
Reverse triiodothyronine (rT3)
- is an inactive form of T3 that is secreted in stress states
Alterations in Thyroid Function
Hyperthyroidism: Thyrotoxicosis
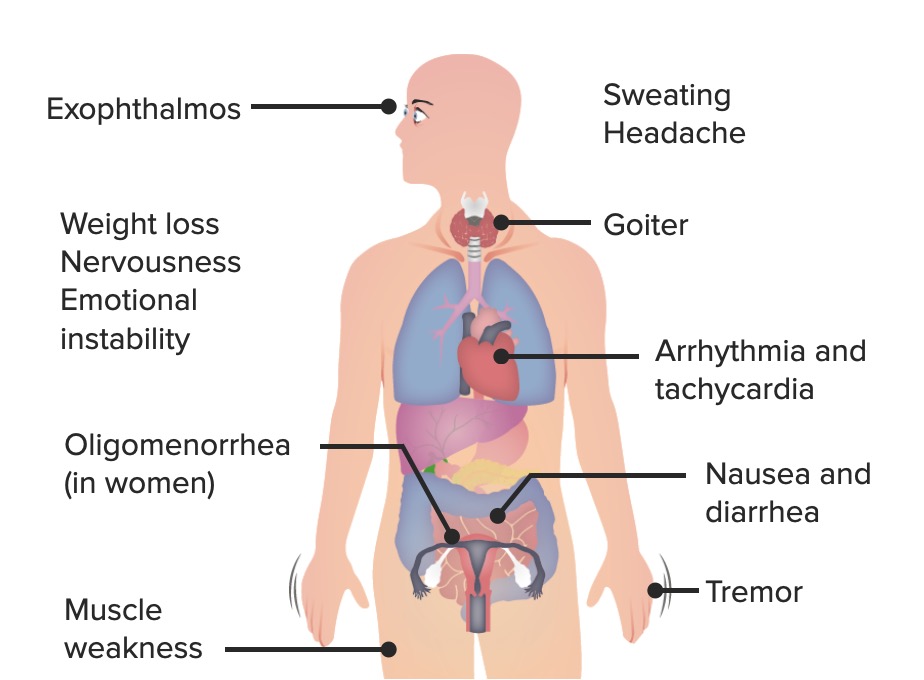
- Is a condition that results from any cause of increased level of thyroid hormone
- Excess amounts of thyroid hormone are secreted from the thyroid gland
- Clinical manifestations
- Increased metabolic rate with heat intolerance
- Increased sympathetic nervous system
- Enlargement of the thyroid gland (goiter)
-
Treatment
- Antithyroid drugs: Methimazole or propylthiouracil (PTU)
- Radioactive iodine therapy: absorbed only by thyroid tissue, causing death of cells
- Surgery
Alterations in Thyroid Function
Hyperthyroidism: Graves Disease
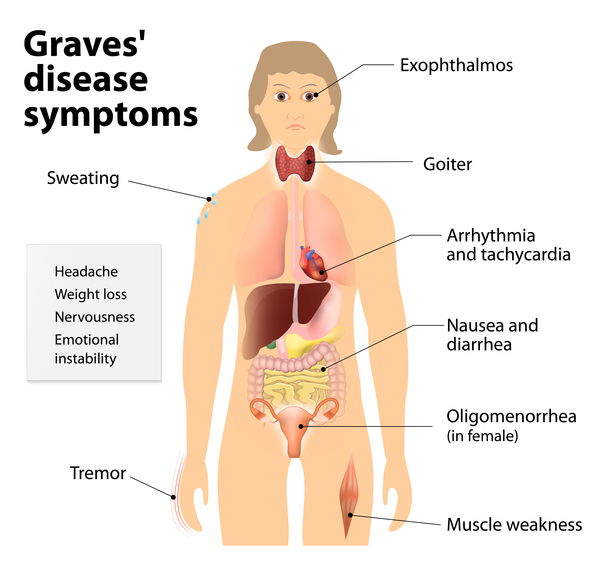
- Is an autoimmune disease
Type II hypersensitivity: infiltration of lymphocytes and thyroid autoantibodies attack TSH receptor and override normal negative feedback mechanisms
-
Clinical
manifestations
- Exophthalmos: increased secretion of hyaluronic acid, orbital fat accumulation, inflammation, and edema of the orbital contents
- Diplopia: double vision
- Ophthalmopathy: enlargement of the ocular muscles,autoimmune inflammatory disorder of the orbit and periorbital tissues,
- Pretibial myxedema (Graves dermopathy): leg swelling; subcutaneous swelling on the anterior portions of the legs and by indurated
-
Treatment
- Antithyroid drugs, radioactive iodine, or surgery
- Does not reverse infiltrative ophthalmopathy or pretibial myxedema
Alterations in Thyroid Function
Hyperthyroidism: Thyroid Storm
- Rare but life threatening within 48 hours if not treated
- Increased action of thyroxine (T4) and triiodothyronine (T3)
- Clinical manifestations
- Hyperthermia
- tachycardia, especially atrial tachydysrhythmias; high-output heart failure
- agitation or delirium
- nausea, vomiting, or diarrhea
-
Treatment I.S.
A.B.C.
- Iodine (saturated solution of
potassium iodide [SSKI])
- iodine blocks the release of T4 and T3 from the gland within hours
- Supportive care
- Antithyroid Drugs: Propyl-thio-uracil or
methimazole
- blocks thyroid hormone synthesis
- Beta-blockers to control cardiovascular symptoms,
- Corticosteroids - reduces the conversion of T4 to T3
- Iodine (saturated solution of
potassium iodide [SSKI])
Alterations in Thyroid Function
Hyperthyroidism: Nodular Thyroid Disease
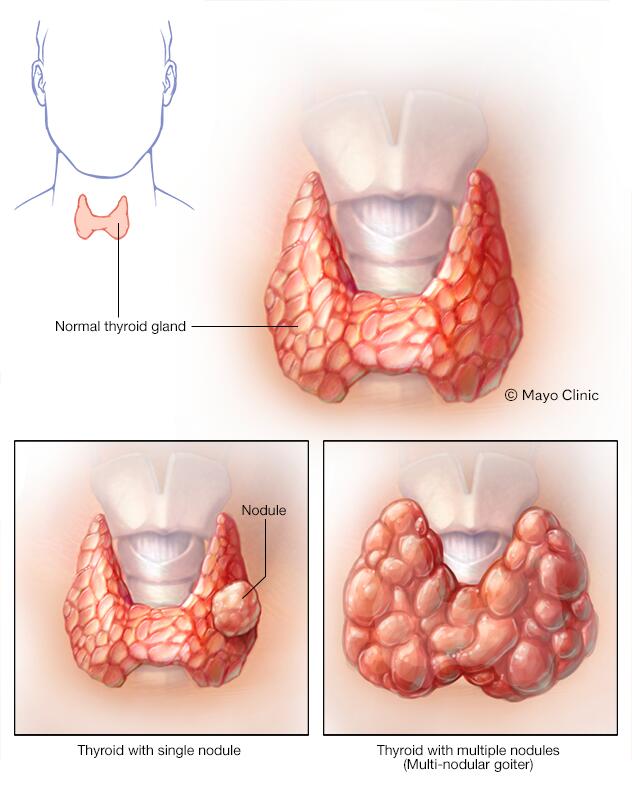
- Hyperthyroidism resulting from nodular thyroid disease
- Toxic multinodular goiter: several hyperfunctioning nodules secrete thyroid hormone
- Solitary toxic adenoma: only one nodule becomes hyperfunctioning
- Clinical manifestations
- Are the same as hyperthyroidism but occur slowly
- Exophthalmos and pretibial myxedema DO NOT occur
-
Treatment
- Must rule out cancer
- Radioactive iodine, surgery, or antithyroid drugs are administered
Alterations in Thyroid Function
Primary Hypothyroidism
What is it?
What are different types?
- Deficient production of thyroid hormone by the thyroid
gland
- Hypothyroidism results from deficient production of TH by the thyroid gland. Hypothyroidism is the most common disorder of thyroid function
Types
- Iodine deficiency (endemic goiter): most common worldwide
- Autoimmune thyroiditis (Hashimoto disease): most common hypothyroidism in the United States
- Postpartum thyroiditis- check post partum women for thyroid levels
Congenital hypothyroidism
What is it?
What can it cause if not treated?
How can it be prevented?
Treatment?
- Present at birth: Due to either: ➢Congenital lack of thyroid gland Or ➢Abnormal making of thyroid hormone
- Thyroid hormone deficiency present at birth
- Consequences if left untreated
- If not treated, Cretinism develops (stunted physical and mental growth due to untreated congenital deficiency of thyroid hormones)
- Prevention
- Neonatal screening to reduce incidents
Treatment
- Administration of T4
- Thyroid carcinoma
- What is the most common cause?
- Characteristics?
- Thyroid carcinoma
- Most common endocrine malignancy from ionizing radiation
- Characteristics
- Changes in voice and swallowing and difficulty in breathing, related to a tumor growth impinging the trachea or esophagus
- Most individuals with thyroid carcinoma have normal T3 and T4 levels
Thyroid cancer typically is discovered as a small thyroid nodule or as a metastatic tumor
diagnostic test: fine needle biopsy of thyroid
S/S of hypothyroidism ?

- Clinical manifestations "3Ls 1D"
- Low basal metabolic rate
- Low basal body temp: cold intolerance
- Low energy: tiredness/lethargy
- Possible Diastolic hypertension
Hypothyroidism
- Myxedema What is it?
- What is myxedema coma? s/s?

-
What is
it
- sign of severe or long-standing hypothyroidism
-
Causes
- Precipitating events include infections, discontinuation of thyroid supplements, overuse of narcotics or sedatives, or a consequence of an acute illness in individuals who have hypothyroidism
S/S
- Myxedema
- Nonpitting, boggy edema, especially around the eyes, hands, and feet; thickening of the tongue
- Medical emergency, diminished level of consciousness
- hypothermia without shivering
- hypoventilation
- hypotension
- hypoglycemia
- lactic acidosis and coma
Hypothyroidism
- Myxedema Treatment
- Treatment
- Levothyroxine (synthetic hormone)
- Myxedema coma
- Thyroid hormone, combined with circulatory and ventilatory support
- Management of hyponatremia and hypothermia
* EXTRA Function of Parathyroid Hormone
- Release of calcium by bones into the bloodstream.
- Absorption of calcium from food by the intestines.
- Conservation of calcium by the kidneys
Alterations in Parathyroid Function
Hyperparathyroidism What is it? Two different causes?
- Excess secretion of PTH
Causes
- Primary hyperparathyroidism
- Excess secretion of PTH from one or more parathyroid glands and hypercalcemia occurs
- 80%–85% caused by parathyroid adenomas
- Secondary hyperparathyroidism
- Increase in PTH, secondary to a chronic disease
- Chronic renal failure
- Dietary deficiency of vitamin D, calcium
- Hypercalcemia does not occur
Alterations in Parathyroid Function
Hyperparathyroidism S/S of primary & secondary & Treatment
- Clinical manifestations
- Primary:
- Most asymptomatic
- Hypercalcemia and hypophosphatemia
- possible kidney stones from hypercalciuria
- alkaline urine
- pathologic fractures bc inc CA leeched out of the bones into the blood
-
Secondary:
- low serum calcium but elevated PTH
- Treatment
- Surgery, bisphosphonates, corticosteroids, and calcimimetics
Alterations in Parathyroid Function
Hypoparathyroidism What is it? Causes?
- Abnormally low PTH levels
- Depressed serum calcium level
- Increased serum phosphate level
- Usual
causes:
- parathyroid damage in thyroid surgery
- autoimmunity
- genetic mechanisms
Alterations in Parathyroid Function
Hypoparathyroidism S/S & Treatment
- Clinical manifestations * S/S of low Ca
- Hypocalcemia
- Muscle spasms/hyperreflexia
- Convulsions
- Laryngeal spasms
- Chvostek and Trousseau signs
- Phosphate retention
- Treatment
- Calcium and vitamin D
- Phosphate binders, if needed