Instructions for Side by Side Printing
- Print the notecards
- Fold each page in half along the solid vertical line
- Cut out the notecards by cutting along each horizontal dotted line
- Optional: Glue, tape or staple the ends of each notecard together
Cardiovascular Part 2
front 1 What is Coronary Artery Disease? | back 1
|
front 2 Most COMMON CAUSE of CAD? | back 2 MOST COMMON CAUSE: Atherosclerosis |
front 3 What are Non Modifiable and Modifiable risk factors for CAD, Myocardial Ischemia, and Acute Coronary Syndromes? | back 3
|
front 4 What is Transient MI? | back 4
|
front 5 Different Types of Angina? | back 5
|
front 6 What is stable angina? Factors that cause ? | back 6
|
front 7 What is Prinzemntal Angina? | back 7
|
front 8 What is Prinzemntal (Variant) Angina? Patho? H.E.A.D. Timing? What is seen on the EKG? | back 8 VAriant Angina- VAsospasms
|
front 9 Prinzemntal (Variant) Angina- Transient MI Treatment ? | back 9 Treatment
|
front 10 What is Unstable Angina? What features does it have?
What does the EKG show? | back 10
AND
*EKG in these patients is typically normal |
front 11 Unstable angina Treatment | back 11
|
front 12 Two types of MI? | back 12  Two major types:
|
front 13 What are structual and functional changes that occur? | back 13
|
front 14 What is Myocardial Infarction? | back 14
|
front 15 Clinical Manifestations of MI? What labs do you look at? | back 15 Myocardial Infarction (cont)
|
front 16 MI Treatment and Complications | back 16 Treatment
|
front 17 What is Acute Coronary Syndrome? Examples of ACS? Complications of ACS? | back 17
|
front 18 ** What are the 4 heart valves? | back 18  |
front 19 What is Valvular Stenosis and Valvular Regurgitation? Valvular disorders are disorders of of the endocardium (the
innermost lining of the heart wall) | back 19 Valvular stenosis
Valvular Regurgitation
|
front 20 What is Aortic Stenosis? What valve is affected? What are S/S? What is treatment? | back 20 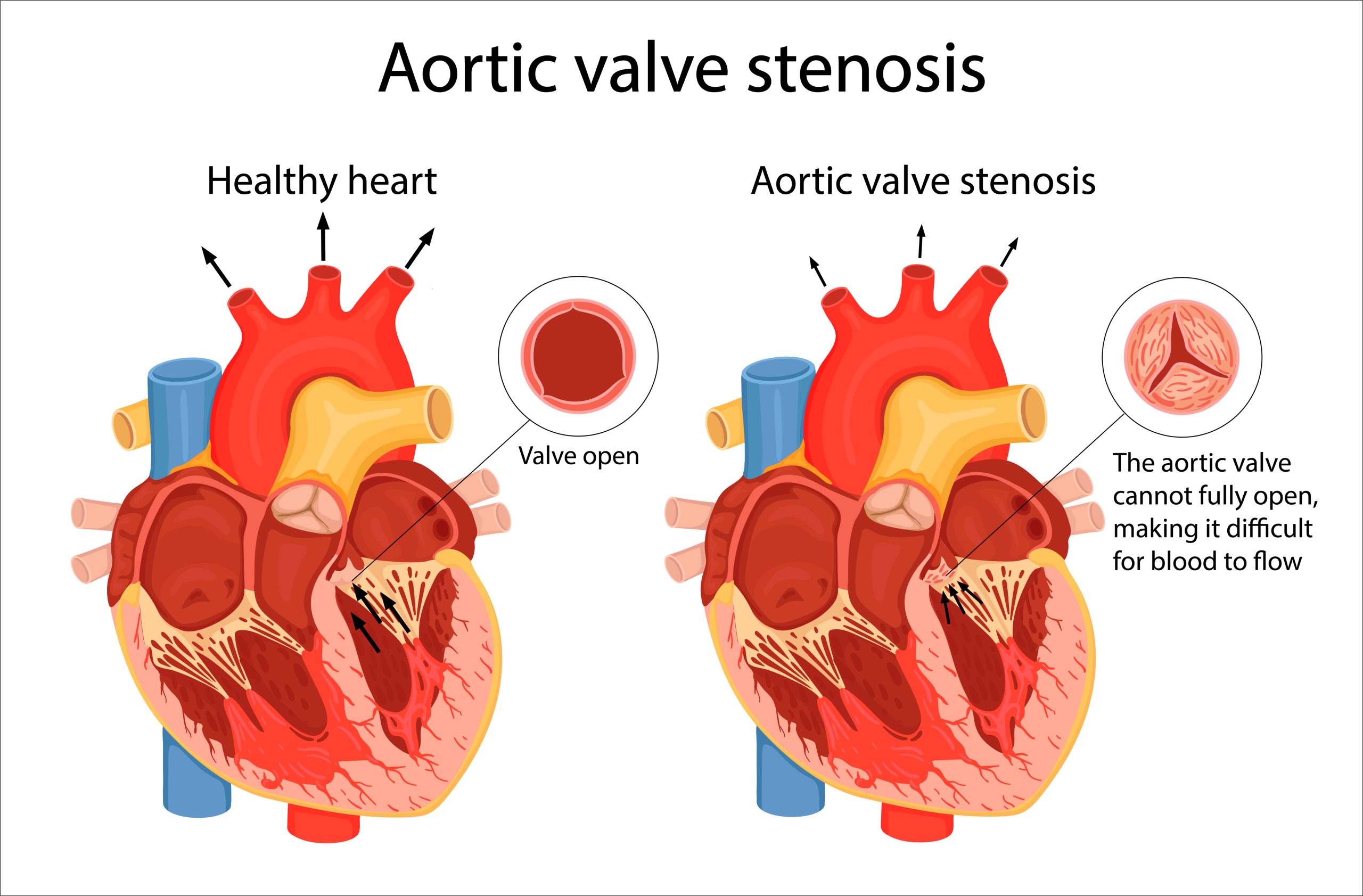 Orifice of the aortic semilunar valve narrows, causing diminished blood flow from the left ventricle into the aorta
|
front 21 What is Mitral Stenosis? Most common cause? What are S/S? What is treatment? | back 21 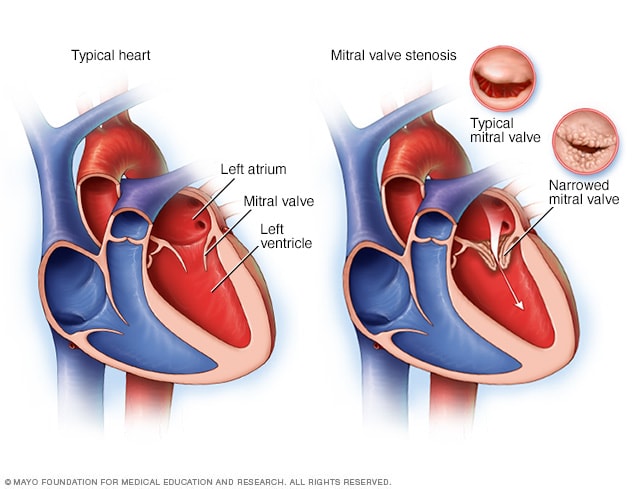 Mitral stenosis
|
front 22 What is Aortic Regurgitation? Causes? S/S? | back 22 
|
front 23 What are Complications of Aortic Regurgitation? What is treatment of Aortic Regurgitation? | back 23 Complications:
Treatment:
|
front 24 Mitral Valve Regurgitation Causes? | back 24
Most common causes
Clinical Manifestations:
Treatment
|
front 25
| back 25
|
front 26 Rheumatic Fever What is it? S/S? Treatment | back 26
|
front 27 Infective Endocarditis What is it? Patho | back 27 
|
front 28 Infective Endocarditis Risk Factors | back 28 P.E.L.V.I.I.C.
|
front 29 Infective Endocarditis S/S | back 29  F.W.C. P.A.T.H.O.J.E.N.
|
front 30 Infective Endocarditis Treatment | back 30 Treatment
|
front 31 Cardiac Terminology Stroke Volume? Cardiac Output? Afterload? Preload? | back 31
(cardiac output = heart rate X stroke volume)
|
front 32 What is Heart Failure ? What are risk factors of heart failure? | back 32 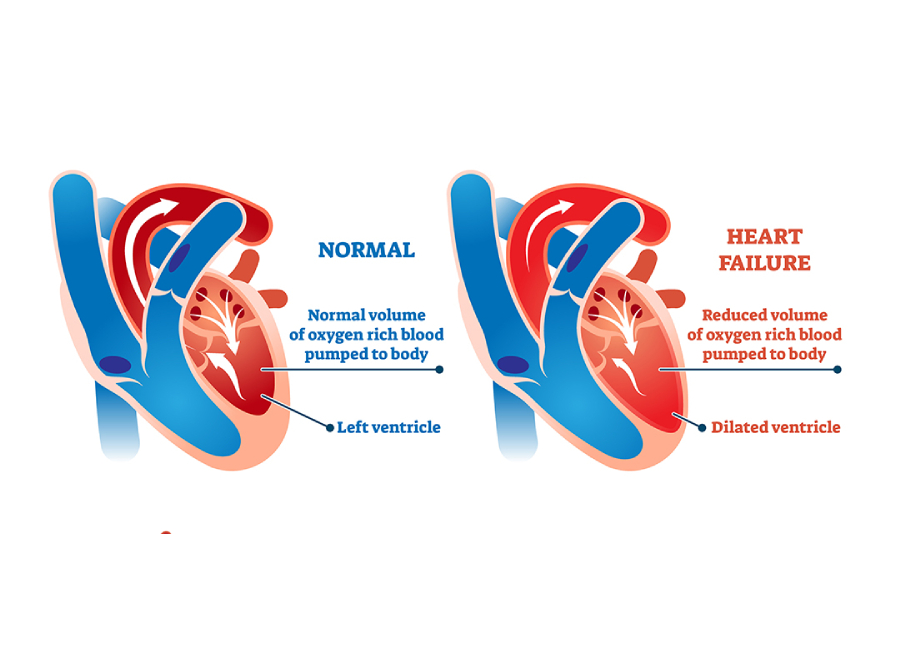
Other risk factors include age, smoking, obesity, diabetes, renal failure, valvular heart disease, cardiomyopathies, myocarditis, congenital heart disease, and excessive alcohol use. |
front 33 What is left sided HF? What can it lead to? think of lungs | back 33 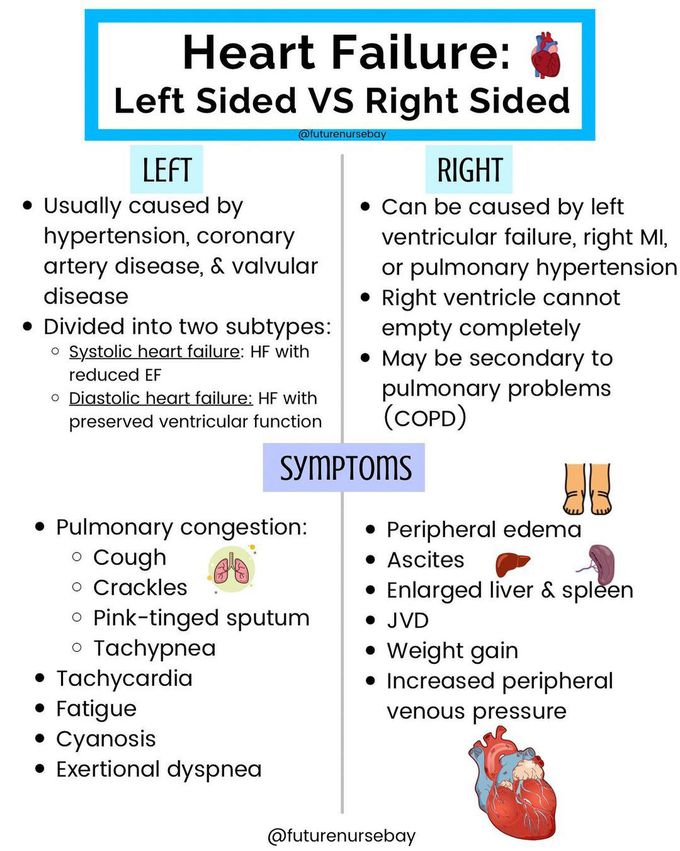
|
front 34 Systolic HF | back 34
These diseases contribute to inflammatory, immune, and neurohumoral changes (activation of the SNS and RAAS) that mediate a process called ventricular remodeling. Ventricular remodeling results in disruption of the normal myocardial extracellular structure with resultant dilation of the myocardium and causes progressive myocyte contractile dysfunction over time |
front 35 Systolic heart failure S/S Systolic HF Treat | back 35
Oxygen, nitrates, and morphine administration improve myocardial
oxygenation and help relieve coronary spasm while lowering preload
through systemic |
front 36 What is Diastolic heart failure S/S? Treatment? | back 36
|
front 37 What is Right Sided HF? What can it cause? | back 37
|
front 38 Right HF S/S? | back 38 Clinical Features: ***(because blood backs up into the systemic venous circulation instead of moving from the right ventricle to the pulmonary circulation)*** E. D.A.S.H.
|
front 39 What are consequences of Heart Failure ? | back 39
|
front 40 Cardiomyopathy What is it? What are they different types? | back 40
|
front 41 Hypertrophic cardiomyopathy What is it? Who does it commonly affect? | back 41
|
front 42 Hypertrophic cardiomyopathy (HCM) S/S? Treatment? | back 42 
Obstruction of left ventricular outflow can occur when heart rate is increased and intravascular volume is decreased
|
front 43 Dilated cardiomyopathy What is it? What are causes? | back 43 
|
front 44 Dilated cardiomyopathy S/S? Treatment | back 44
|
front 45 Restrictive cardiomyopathy What is it? Causes? | back 45
myocardium becomes rigid and noncompliant, impeding
ventricular
|
front 46 Restrictive cardiomyopathy S/S? Treatment? | back 46
|
front 47 Atrial Fibrillation What is it? Causes? S/S? Treatment? | back 47
β-blockers usually act to modulate the activity of the SA and AV nodes |
front 48 Infants: Congenital Heart Disease | back 48
|
front 49 Defects With Increased Pulmonary Blood Flow Patent ductus arteriosus (PDA) What is it? S/S? Treatment? | back 49 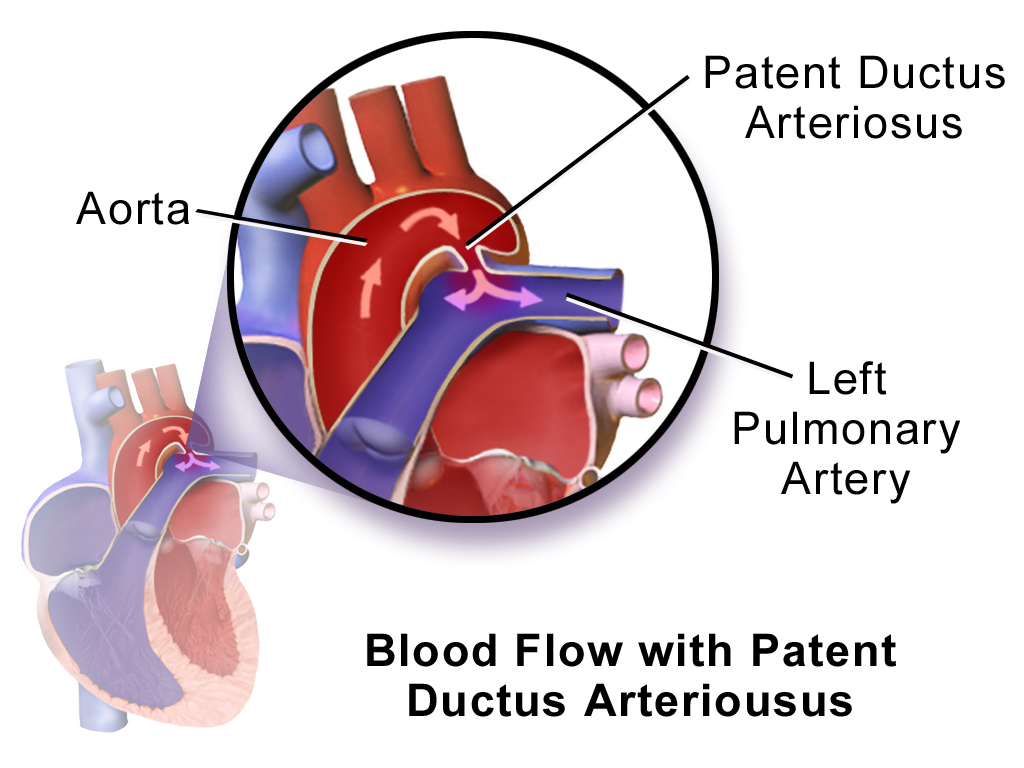
|
front 50 Defects With Increased Pulmonary Blood Flow
What is it? S/S? Treatment? | back 50 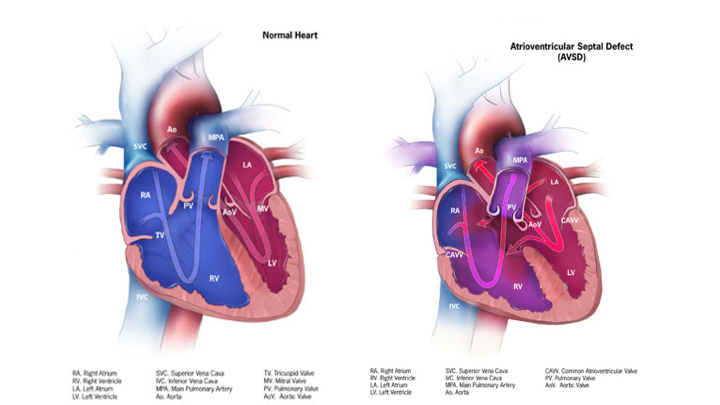
|
front 51 Defects With Increased Pulmonary Blood Flow
What is it? S/S? Treatment? | back 51 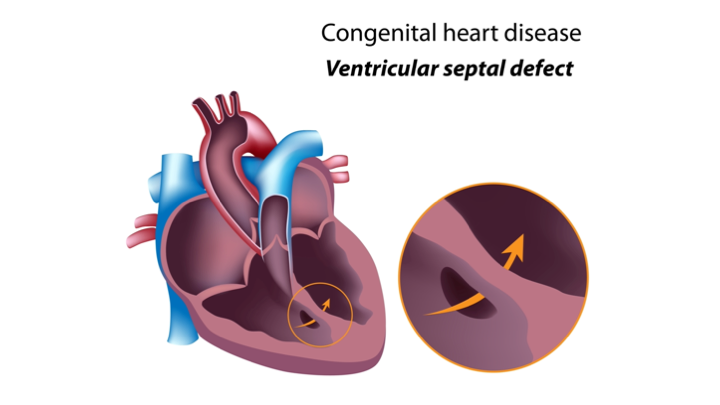
|
front 52 Defects With Decreased Pulmonary Blood Flow: Tetralogy of Fallot What is the defect? S/S? Treatment | back 52 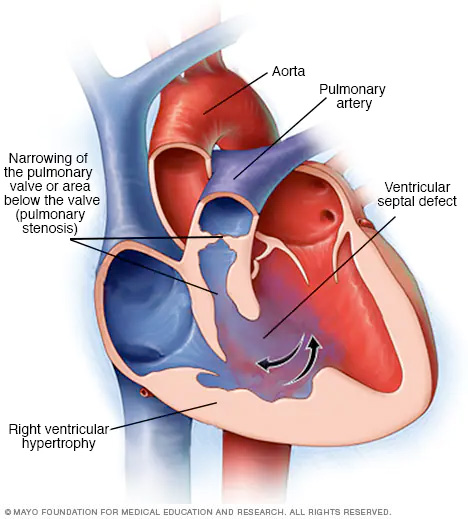
|
front 53 Obstructive Defects: Coarctation of the Aorta | back 53 
|
front 54 Obstructive Defects: Coarctation of the Aorta S/S? Treatment? | back 54
|
front 55 Obstructive Defects: Hypoplastic Left Heart Syndrome | back 55 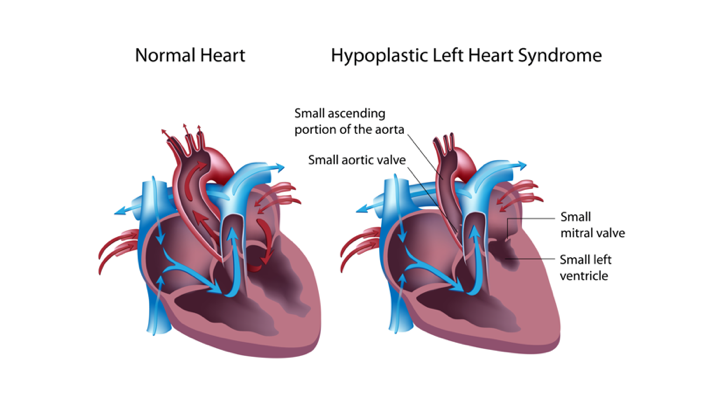
|
front 56 Mixing Defects: Transposition of the Great Arteries | back 56 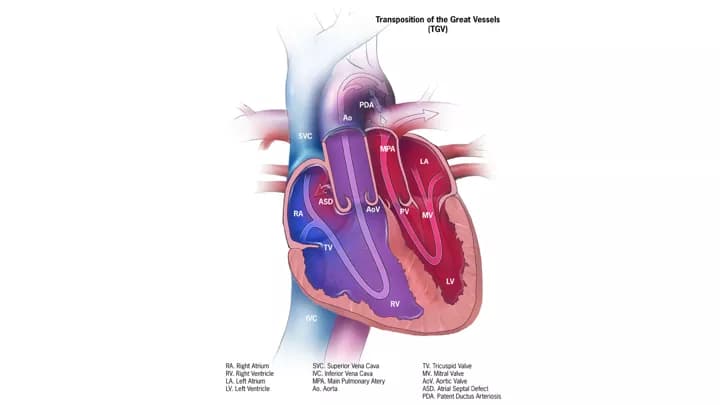
|