What does TEP stand for
Totally Extraperitoneal Patch
•Class 1: Clean
What is a surgical procedure that is performed to correct a hiatal hernia

Laparoscopic Nissen Fundoplication
•Class 1: Clean
Who inserts the bougie dilator for a Laparoscopic Nissen Fundoplication because they cannot be passed from the sterile field
Anesthesia
What can also treat gastroesophageal reflux disease (GERD)as well as a hiatal hernia
Laparoscopic Nissen Fundoplication
Laparoscopic Nissen Fundoplication unique supplies
Abdominal Lap drape
Maloney (bougie dialators)
#11 and #15 blades
What occurs when the esophageal hiatus is weak, which allows the abdominal esophagus and superior portion of the stomach to protrude into the thoracic cavity.
Hiatal hernia
What surgery does the surgeon wraps (plicates) the top of the stomach (fundus) around the bottom of the esophagus and stitches it in place (wrap)
Laparoscopic Nissen Fundoplication
What is the surgical creation of an opening (fistula tract) from the gastric mucosa to the skin and is performed to provide nutrition “feeding” to the patient or to decompress and drain the stomach
A gastrostomy
•Class II: Clean-contaminated
What is the timeline for a gastrostomy
Long term or temporary depending on technique and condition
What are the layers of the stomach:
Serosa
Muscle
Submucosa
Mucosa

serosa
What is the main purpose of a gastrostomy
Create an opening to bypass the esophagus
What type of suture pattern do they use for a PEG procedure
Pursestring
Often tumors of the larynx, pharynx, esophagus, and proximal stomach, as well as esophageal stricture, dictate the timeline for a .........
A gastrostomy
What are the ways a gastrostomy can be created
Open
Percutaneous
Endoscopic
Laparoscopic
What gastrostomy is a surgically placed feeding tube in the stomach
Stamm Gastrostomy
Usually performed through a small (6-8 cm) upper midline incision
What does PEG stand for
Percutaneous Endoscopic Gastrostomy
Push method
What type of feeding tube is used for patients on a ventilator, who may have a spinal cord injury, dementia, or cerebral palsy

Percutaneous Endoscopic Gastrostomy
What is a tube that is passed through the nose and down through the nasopharynx and esophagus into the stomach
Nasogastric tubes
What is the removal of part or all of the stomach

Gastrectomy
What is the surgical removal of the distal portion of the stomach and the pylorus
Reanastomosis is to the duodenum

Gastroduodenostomy Billroth I
(Picture A)
What is the surgical removal of the distal portion of the stomach and the pylorus.
Reanastomosis is to the jejunum

Gastrojejunostomy Billroth II
(Picture B)
Stomach anatomy

What involves removal of the stomach and re-constitution of the alimentary tract

Total gastrectomy
•Class II: Clean-contaminated
What requires an upper midline incision, bilateral subcostal incision (chevron), or thoracoabdominal incision
Total gastrectomy
When doing abdominal cases what is the best technique to employ
Bowel technique
What is a term used to describe the contraction of the muscles that mix and propel contents in the gastrointestinal tract
Motility disorders
Pathology of the Esophagus - what causes
•Dysphagia
•Regurgitation of undigested food
Motility disorders
What is a disease of the muscle of the esophagus
Achalasia
What is a condition where the pea-sized, bulging pouches in the inner lining of the bowel become inflamed

Diverticulitis
What is the medical or biological term for an outpouching of a hollow (or a fluid-filled) structure in the body
Diverticula
What is connected to the lesser curvature of the stomach and extends to the posterior surface of the liver to hold the stomach in place.
The lesser omentum
What extends from the diaphragm to the cardia of the stomach to also help keep the stomach in normal anatomic position
The gastrophrenic ligament
What is the inferior border of stomach called
The greater curvature.
What is the attachment of two ends of approximately the same sized structures
2 layer closure technique with sutures or staples

End-to-end anastomosis
What is the attachment of the end of one section of bowel into the side of another section (T-like)
Not used that often, if so typically in patients with multiple revisions, or cancer patients

End-to-side anastomosis
What is the creation (attachmen) of parallel opening in two sections of bowel with anastomosis
2 different sizes coming together
parallel opening

Side-to-side anastomosis
What is a specific technique of anastomosis that allows for a variety of applications in gastric, intestinal, biliary, and pancreatic surgery often referred to as gastric bypass

Roux-en-Y
Attaches to duodenum
What is inspected to ensure good blood flow to the remaining segments of bowel

The mesentery
(being inspected for blood flow)
The mesentery is a fold of membrane that attaches the intestine to the abdominal wall and holds it in place

The mesentery
An elevated white blood cell count and fever are common symptoms for
Appendectomy
After which surgery are all instruments placed in a basin and removed from the immediate field. The basin is placed in a predefined area on the back table and left there until the case is completed. Instruments and needles are counted by pointing, not by touching. This includes any specimens removed
Appendectomy
•Class 2: Clean-contaminated
Where are the appendix located
Right lower quadrant
What incision is used for an open appendectomy
McBurney's
After the appendix has been removed what suture is used and procedure performed to the stump
Stump is sutured with a purse string suture and inverted inside itself
Appendectomy:
(A) Cecum and appendix identified,
(B) mobilization of appendix
(C) appendiceal artery ligated,
(D) excision of appendix

What is the anatomy of the colon:
Cecum
Ascending colon
Transverse Colon
Descending Colon
Sigmoid Colon
Rectum
Anal Canal

What begins at hepatic flexure, travels across top of abdominal cavity, and ends at splenic flexure
Transverse colon
What occurs (in toddlers) when a portion of the intestine folds inside another part. This causes a blockage in the colon

Intussusception
Colon resection options:
(A) Right colectomy,
(B) right hemicolectomy,
(C) transverse colectomy,
(D) left colectomy,
(E) left hemicolectomy,
(F) abdominoperineal resection

What is a section of bowel that communicates with the outside of the abdominal cavity that is created to divert the fecal stream
A stoma (“ostomy”)
What is a surgically created opening to divert feces to the outside temporarily or permanently
A Stoma
What are created from either an end section or loop of the ileum (ileostomy) or colon (colostomy).

Stomas
What is the name for the colostomy that the bowel is pulled out onto the abdomen and held in place with an external device. The bowel is then sutured to the abdomen and two openings are created in the one stoma: one for stool and the other for mucus.
Loop colostomy (Diversion)
What is the name for the stoma that is created from one end of the bowel. The other portion of the bowel is either removed or sewn shut
End colostomy (End)
Hartmann's procedure
What is constructed from a terminal portion of ileum, can be temporary or permanent
End ileostomy
What is primarily a TEMPORARY stoma for fecal diversion
Loop ileostomy
What is a modification of the loop method in which the loop is divided with a linear cutter and both ends are brought out through the skin incision
End-loop ileostomy
What is created from the descending COLON and sigmoid
End colostomy
What utilizes the transverse COLON
•Not generally used as a permanent colostomy because it discharges a semiliquid stool
•The most frequently used method of stoma creation for temporary fecal diversion
Loop colostomy
What is a modification of the loop method in which the loop is divided with a linear cutter and both ends are brought out through the skin incision
End-loop colostomy
What is the most common type of permanent colostomy
•Created at the time of A/P resection
•Created as an end colostomy in the lower left quadrant
Sigmoid colostomy
What is a chronic form of perianal abscess that fails to heal after draining and becomes an inflammatory tract

Fistula-in-ano
What is a tear in the lining of the lower rectum
Anal fissure
What is a cyst or abscess near or on the natal cleft of the buttocks that often contains hair and skin debris

Pilonidal disease
What are the most common anal lesions, can be internal or external vascular structures in the anal canal

Hemorrhoids
What is the membranous layer of subcutaneous tissue of the abdomen, it is attached to iliac crest, linea alba, pubis

Scarpa’s fascia
What separates aponeurosis of external oblique muscle from overlying tissues and contains the intercrural fibers
Interparietal fascia
What separates aponeurosis of external oblique muscle from overlying tissues and contains the intercrural fibers
Innominate fascia
What is a thin layer of fascia lining the transversus abdominis muscle
Transversalis fascia
Where do we see the following fascia:
Scarpa’s fascia
Innominate fascia
Interparietal fascia
Transversalis fascia
McVay (Cooper Ligament) Inguinal Herniorraphy
What is an anatomic triangle formed by cystic duct, common hepatic duct, and inferior borderof liver; used to locate the cystic artery, which is usually within the triangle
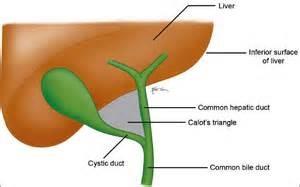
Triangle of Calot
What is performed for managing tumors of the head of the pancreas, the most common site of pancreatic cancer
The Whipple procedure
What is the medical name for a Whipple
Resection is an en bloc excision of the head of the pancreas, the distal one-third (antrum and pylorus) of the stomach, all of the duodenum, the proximal 10 cm of the jejunum, the gallbladder, the cystic and common bile ducts, and the peripancreatic and hepatoduodenal lymph nodes

Pancreaticoduodenectomy
What is the surgical cutting of the vagus nerve to reduce acid secretion in the stomach

Vagotomy
Mouth
The Pharynx and Esophagus
The Stomach and Small Intestine
The Colon (Large intestines), Rectum, and Anus
Basic steps through the alimentary canal
What is the largest parenchymal organ in the abdominal cavity
Liver
It's function is to reabsorb fluids and process waste products
Colon
What organ is the single largest mass of lymphatic tissue in the abdominal cavity
Spleen
What organ is responsible for both the storage and purification of red blood cells
Spleen
What means in a direction towards the head
Cephalad
What means in a direction towards the feet
Caudal
What is the semifluid mass of partly digested food that is expelled by the stomach into the duodenum
Chyme
What is a solid mass of indigestible material that accumulates in your digestive tract, sometimes causing a blockage
Bezoar
What is difficulty swallowing
Dysphagia