Blood
- Transports essential oxygen to tissues along with nutrients required for cellular metabolism
- provides for the necessary removal of many cell wastes
- plays a critical role in the body's defenses/immune system
- serves in maintaining body homeostasis
- Provides a mechanism for controlling body temperature by distributing Core heat throughout the peripheral tissues
Two Separate Circulations
- The pulmonary circulation
- The systemic circulation
The Pulmonary Circulation

- allows The exchange of oxygen and carbon dioxide in the lungs
The Systemic Circulation

- Provides for the exchange of nutrients and wastes between the blood and the cells throughout the body
Arteries

- Transports Blood away from the heart
Arterioles

- The smaller branches of arteries
- Controls the amount of blood flowing into the capillaries in specific areas through the degree of contraction of smooth muscle in the vessel wall
Capillaries

- Very small vessels
- Forms the microcirculation
- Blood flow very slowly through capillaries
- precapillary sphincters
- Single
endothelial layer
- Facilitates the exchange of fluid, oxygen, carbon dioxide, electrolytes glucose, and other nutrients and waste between the blood and interstitial fluid
Precapillary Sphincters
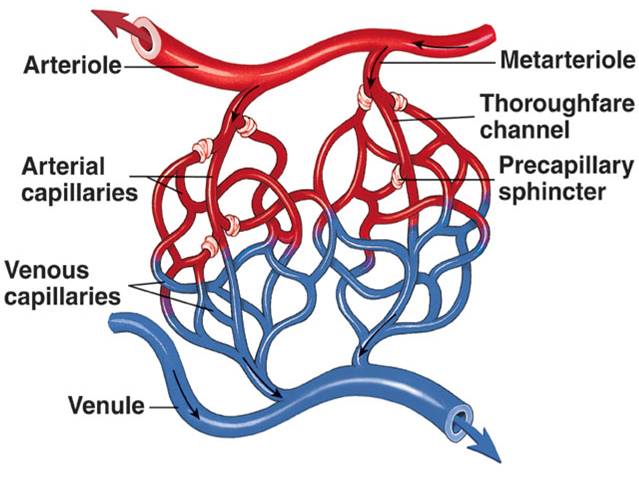
- Determines the amount of blood flowing from the arterioles into the individual capillaries
- depends on the metabolic needs of the tissues
Small Venules
- conduct blood from the capillary beds toward the heart
Veins
- returns blood back to the heart
- Have thinner walls than arteries and less smooth muscles
Capacitance Vessels
- the blood vessels that hold the major portion of theintravascular blood volume
- veins
Walls of arteries and veins

-
Tunica Intima
- the inner layer
- endothelium (simple squamous)
- flat so fluid can be exchanged back-and-forth
-
Tunica Media
- The middle layer
- Layer of smooth muscle
- Controls the diameter and lumen size
-
Tunica Adventitia
- outer connective tissue layer
- Contains elastic and collagen fibers
autoregulation
- A reflex adjustment in a small area of a tissue
- varies depending on the needs of the cells in the area
Causes of local vasodilation
- decrease in pH
- increase in carbon dioxide
- decrease in oxygen
composition of blood

- Water and its dissolve solutes (plasma) = 55% of the whole blood volume
- remaining 45% is composed of the cells or formed elements erythrocytes, leukocytes, and thrombocytes
Hematocrit

- Refers to The proportion of cells in blood
- Indicates the viscosity of the blood
plasma

- The clear yellowish fluid remaining after the cells have been removed
-
contains:
- water 92%
- plasma proteins 7%
- other solutes 1%
- Amino acids
- Carbohydrates
- Lipids
- Vitamins
- Hormones
- Enzymes
- Electrolytes
- Wastes
serum

- Refers to the fluid and solutes remaining after the cells and fibrinogen has been removed
Examples of plasma proteins
- Albumin
- Globulins/Anti-bodies
- fibrinogen
albumin
- Maintains osmotic pressure in the blood
Fibrinogen
- essential for the formation of blood clots
Red bone marrow
- Origination of all blood cells
- found in the flat and irregular bones, ribs, vertebrae, sternum, and pelvis
Erythrocytes or red blood cells
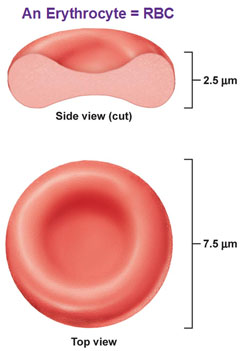
- Biconcave flexible discs
- non-nucleated when mature state
- Contain hemoglobin
- Size and structure are essential for easy passage to small capillaries
- life span = 120 days b/c no nucleus
Erythropoietin
- Originates in the kidney
- Hormone that stimulates erythrocyte production in the red bone marrow
Hemoglobin

-
Consists of:
- the globlin portion
- two pairs of amino acid chains
- four
heme groups
- each containing a ferrous iron atom, to which oxygen molecule can attach
- the globlin portion
Oxyhemoglobin
- A bright red color that distinguishes arterial blood from venous blood
deoxyhemoglobin
- Dark bluish red in color and font and venous blood
Leukopoiesis
- Production of white blood cells
- Stimulated by colony stimulating factors that are produced by cells such as macrophages and T lymphocytes
leukocytes
- Makes up only about 1% of blood volume
- Subdivided into
two categories:
- Granulocytes
- Agranulocytes
- All types develop in differentiate from the original stem cell in bone marrow
- There are five types of leukocytes
- Lymphocytes
- Neutrophils
- Basophils
- Eosinophils
- Monocytes
Lymphocytes
- Makes up 30 to 40% of the white blood cells
neutrophils
- The most common leukocyte
- Makes up 50 to 60% of White blood cells
- Survive only four days
- The first to respond to any tissue damage And phagocytosis
- Increase in numbers by bacterial affection
Basophils
- Can release histamine and heparin
- Maybe fixed in tissues or wandering
Eosinophils
- Combat the effects of histamine
- Increase by allergic rea ctions and parasitic infections
monocytes
- can enter the tissue to become macrophages
differential count
- Indicates the proportion the specific types of white blood cells in the blood
- Assist in making a diagnosis
Thrombocytes
- Essential part of the blood clotting process
- Not cells
- Non-nucleated
Hemostasis (3 steps)
- An immediate response of a blood vessel to injury is vasoconstriction of vascular spasm
- Form a platelet plug in the vessel
- Coagulation mechanism
Heparin
- an anticoagulant
- Released from basophils or mast cells in the tissues
- Blocks thrombin
- Does not dissolve clots but prevents further growth of the thrombus
Blood type
- Determined by the presence of specific antigens on the cell membranes of erythrocytes
ABO groups
- An inherited characteristic
- Depends on the presence of type A or B antigens
type O blood
- Lack A and B antigens
- are considered universal donors
type A and B blood
- Are universal recipients
RH system
- May cause blood and incompatibility if the mother is Rh negative and the fetus is Rh positive
- Antigen D in plasma membrane = RH positive
- Absence of antigen D = RH negative
Complete blood count (CBC)
diagnostic test for blood
- Includes total red blood cells, white blood cells, platelet count, and morphology (size and shape), a differential count for white blood cells, hemoglobin, and hematocrit values
Leukocytosis
- An increase in white blood cells
- Often associated with inflammation or infection
leukopenia
- Decrease in leukocytes
- Occurs with some viral infections as well as with radiation and chemo therapy
increase in eosinophils
- Common with allergic responses and parasitic infections
morphology
- Observe with blood sMears
- Shows size, shape,
uniformity, and maturity of cells
- Helps to distinguish different types of anemia
Hemoglobin (diagnostic test)
- Amount of hemoglobin per unit volume of blood
- Mean
corpuscular volume
- Indicates the oxygen-carrying capacity of blood
- Mean corpuscular hemoglobin
Reticulocyte Count
- Assessment of bone marrow function
Chemical analysis of the blood
- Determine serum levels of components such as iron, vitamin B12, folic acid, cholesterol, urea, and glucose
Bleeding time (diagnostic test)
- Measures platelet function
prothrombin time (PT) and partial thromboplastin time (PTT)
- Measures function of various factors in coagulation process
- interNational normalized ratio is a standardized version
partial thromboplastin time
- Measures the intrinsic pathway
- PTT... the 2 t's are in(trinsic) a relationship
prothrombin time
- measures the extrinsic pathway
anemia
- A reduction in oxygen transport in the blood due to a decrease in hemoglobin content
- May result from the declining production of the protein, a decrease in the number of erythrocytes, or a combination of these factors
- May be classified by typical cell morphology
-
oxygen deficiency leads to:
- Less energy production and all cells
- Cell metabolism and reproduction diminished
- Compensation mechanism to improve the oxygen supply
- ex:
- Tachycardia
- peripheral vasoconstriction
- ex:
- General signs of anemia
- Fatigue, Pallor, dyspnea, and tachycardia
- Decrease regeneration of epithelial cells
- Less energy production and all cells
Iron deficiency anemia
- Insufficient iron impairs hemoglobin synthesis
- Which reduces the amount of oxygen transported in the blood
- Red blood cells are microcytic and hypochromic
- Very common
- Ranges from mild to severe
- Occurs in all age groups
- One in five women is affected
- Proportion increases for pregnant women
- Frequently a sign of an underlying problem
Etiology of iron deficiency anemia
- Dietary intake of iron may be below the minimum requirement
- Chronic blood loss
- duodenal absorption of iron may be impaired
- Severe liver disease may affect both iron absorption and iron storage
Manifestations of iron deficiency anemia
- pallor of the skin and mucous membranes
- Due to vasoconstriction
- Fatigue,lethargy, and cold intolerance
- b/c cell metabolism decreased
- Irritability
- A central nervous system response to hypoxia
- Degenerative changes
- such as brittle hair, spoon shaped and rigid nails
- Inflammation of oral mucosa and tongue
- Menstrual irregularities
- Delayed healing
- Tachycardia, heart palpitations, dyspnea, syncope
* People who have iron deficiency anemia may have unusual craving for nonfood items such as ice, paint, or starch. This craving is called pica
Diagnostic tests for Iron deficiency anemia
- Laboratory test demonstrate low values of hemoglobin, hematocrit, mean corpuscular volume and mean corpuscular hemoglobin, serum ferritin and serum iron, and transferrin saturation
Treatment for iron deficiency anemia
- Identified underlying cause and resolves if possible
- Consume Iron rich foods or iron supplements
pernicious anemia: vitamin B12 deficiency (megaloblastic anemia)
- The common form of megaloblastic anemia
- Caused by the malabsorption of the vitamin B12
- Iron deficiency may be present as well
- Red blood cells are very large and contain nuclei
- Dietary and sufficiency is a very rare cause
- May be an outcome of surgeries in which the parietal cells are removed or resection of the ileum which is a sight of absorption
Vitamin B12 and nerve cells
- Vitamin B12 is needed for the function and maintenance of neurons
- Deficiency can result in neuropsychiatric symptoms
Manifestations of pernicious anemia
- Tongue is typically in large, red, sore, and shiny
- Decrease in gastric acid leads to digestive discomfort such as nausea and diarrhea
- Tingling or burning sensations in the extremities or loss of coordination and ataxia
Diagnostic tests for pernicious anemia
- Microscopic examination (erythrocytes)
- Bone marrow examination (hyperactive)
- Vitamin B12 serum levels below normal
Treatment for Pernicious Anemia
- Oral supplements are recommended
- Vitamin B12 is administered by injection
Aplastic anemia
- Results from impairment or failure of bone marrow leading to loss of stem cells and pancytopenia
- may be temporary or permanent
- often idiopathic
Pancytopenia
- decreased numbers of erythrocytes, leukocytes, and thrombocytes in the blood.
Hemolytic Anemia
- results from excessive destruction of RBCs
- leads to a low erythrocyte count and low hemoglobin
-
causes:
- genetic defects
- immune reactions
- Changes in blood chemistry
- Presence of toxins in the blood
- Infections such as malaria
- Antigen-antibody reaction
- Incompatible blood transfusion
What term is used to describe a deficit of all types of blood cells?
- Leucopenia
- Neutropenia
- Pancytopenia
- Erythrocytosis
- PANCYTOPENIA
Capillary walls consist of:
- multiple endothelial layers.
- a thick layer of smooth muscle.
- two or three epithelial layers.
- a single endothelial layer
- a single endothelial layer
Individuals with type O blood are considered to be universal donors because their blood:
- contains A and B antibodies.
- contains A and B antigens.
- lacks A and B antibodies.
- lacks A and B antigens.
- lacks A and B antigens.
What causes numbness and tingling in the fingers of individuals with untreated pernicious anemia?
- Persistent hyperbilirubinemia
- Increasing acidosis affecting metabolism
- Vitamin B12 deficit causing peripheral nerve demyelination
- Multiple small vascular occlusions affecting peripheral nerves
- Vitamin B12 deficit causing peripheral nerve demyelination
What is the cause of oral ulcerations and delayed healing occurring with any severe anemia?
- Lack of folic acid for DNA synthesis
- Frequent microinfarcts in the tissues
- Deficit of oxygen for epithelial cell mitosis and metabolism
- Elevated bilirubin levels in blood and body fluids
- Deficit of oxygen for epithelial cell mitosis and metabolism
Why is pernicious anemia treated with injections of vitamin B12?
- An immune reaction in the stomach would destroy the vitamin.
- Digestive enzymes would destroy the vitamin.
- The vitamin irritates the gastric mucosa.
- The ingested vitamin would not be absorbed into the blood.
- The ingested vitamin would not be absorbed into the blood.
Why do vascular occlusions and infarcts occur frequently with sickle cell anemia?
- The red blood cells are abnormally large.
- Increased hemolysis of erythrocytes occurs.
- Erythrocytes change to sickle shape when hypoxia occurs
- HbS is unable to transport oxygen
- Erythrocytes change to sickle shape when hypoxia occurs
In cases of polycythemia vera, blood pressure is elevated as a result of:
- increased blood volume.
- frequent infarcts in the coronary circulation.
- congested spleen and bone marrow.
- increased renin and aldosterone secretions.
- increased blood volume.
In individuals with pernicious anemia, antibodies form to:
- vitamin B12 .
- intrinsic factor or parietal cells.
- mucus-producing glands.
- hydrochloric acid.
- intrinsic factor or parietal cells.
Petechiae and purpura are common signs of:
- excessive hemolysis.
- leucopenia.
- increased bleeding.
- hemoglobin deficit.
- increased bleeding.
Which of the following substances acts as an anticoagulant?
- Prothrombin
- Heparin
- Fibrinogen
- Vitamin K
- Heparin
Why is excessive bleeding a common occurrence with acute leukemia?
- Deficit of calcium ions
- Impaired production of prothrombin and fibrinogen
- Decreased platelets
- Dysfunctional thrombocytes
- Decreased platelets
Multiple myeloma is a malignant tumor involving:
- plasma cells.
- granulocytes
- bone cells.
- lymph nodes.
- plasma cells.
The Reed-Sternberg cell is diagnostic for:
- chronic myeloblastic leukemia.
- Hodgkin’s lymphoma.
- multiple myeloma.
- non-Hodgkin’s lymphoma.
- Hodgkin’s lymphoma.
Which of the following applies to the leukemias?
- Chronic leukemias are more common in older people.
- AML is the most common childhood leukemia.
- Exposure to chemicals is not considered a predisposing factor.
- Lymphoid tissue produces abnormal leukocytes.
- Chronic leukemias are more common in older people.
A high percentage of blast cells in the leukocyte population indicates a poor prognosis for an individual with:
- thalassemia
- acute myelogenous leukemia (AML).
- myelodysplastic syndrome.
- multiple myeloma.
- acute myelogenous leukemia (AML).
Which of the following applies to erythropoietin?
- It is produced by the liver.
- It increases iron absorption for heme production.
- It stimulates production of red blood cells.
- Hypoxia stimulates the red bone marrow to produce erythropoietin.
- It stimulates production of red blood cells.
Microcytic and hypochromic erythrocytes are commonly found as a result of:
- iron deficiency anemia.
- polycythemia
- disseminated intravascular coagulation.
- hemophilia A
- iron deficiency anemia.