What is the difference between sensitivity and specificity
What does it mean?
Sensitivity
- Sensitivity is the probability that a person with disease has a positive test.
- Sensitivity is also known as the true positive rate
- SENSITIVE TEST WITH NEGATIVE RESULT= RULES OUT DISEASE
Specificity
- Specificity is the probability that a non diseased person has a negative test,
- Specificity is also known as the true negative rate.
- SPECIFIC TEST WITH POSITIVE RESULTS= RULES IN DISEASE
What are clues in patient history or clinical manifestations that may indicate eating disorder?
Clinical Manifestations
- Excess clothing
- Decreased food intake
- Loss of appetite
- Excessive physical activity
- Abnormal, obsessive, or ritualized eating behaviors.
- History of eating disorders in family
- Bullying regarding weight
How do you take proper BP for most accuracy?
- Measure blood pressure using a sphygmomanometer.
- Select the appropriate blood pressure–measuring device.
- Prepare the patient and setting.
- Select the correct size blood pressure cuff.
- Position the arm and cuff appropriately.
- Use the palpated radial pulse obliteration pressure to estimate systolic blood pressure.
- Position the stethoscope diaphragm or bell over the brachial artery.
- Inflate the cuff rapidly to target level followed by gradual deflation.
- Identify systolic and diastolic blood pressures.
- Average two or more readings.
- Measure blood pressure in both arms at least once
- If the cuff is too small (narrow), the blood pressure will read high
- If the cuff is too large (wide), the blood pressure will read low on a small arm and high on a large arm.
Recognize the S&S of depression?
personal history of a depressive episode, a family history of first-degree family members with depression, personal history of recent stressful life events or significant childhood adversity, chronic and/or disabling medical illness, and female gender
S/S
- crying
- pacing
- hand-wringing of agitated depression or anxietY
- the hopeless, slumped posture and slowed movements of depression
- impaired recent memory
- low self-esteem, loss of pleasure in daily activities (anhedonia), sleep disorders, and difficulty concentrating or making decisions.
Risk factors of suicide?
- Risk Factors:
- include presence of a mental health disorder
- serious adverse childhood events
- family history of suicide
- prejudice or discrimination associated with being lesbian, gay, bisexual, or transgender
- access to lethal means
- possibly a history of being bullied
- sleep disturbances
- chronic medical conditions
- MEN- socioeconomic factors, low income
- OLDER ADULTS-social isolation, spousal bereavement, neurosis, affective disorders, physical illness, and functional impairment
- MILITARY- TBI, PTSD, DC from military service in past 12 months
- If you suspect depression, assess its severity and any risk of suicide. Ask: Do you feel discouraged or depressed?How low do you feel?What do you see for yourself in the future?Have you had thoughts of death?Do you ever feel that life isn’t worth living? Or that you want to be dead?Have you ever thought of killing yourself?Have you thought about how or when you would try to kill yourself? Do you have a plan?What do you expect is going to happen after you die?It is your responsibility to ask directly about suicidal thoughts. This may be the only way to uncover suicidal ideation and plans that launch immediate intervention and treatment.
- USPSTF has concluded that the current evidence is insufficient to assess the balance of benefits and harms of screening for suicide risk in a primary care setting
What is the relationship between substance abuse and depression/anxiety?
About 16 million adult Americans, or almost 7%, have major depression, often with coexisting anxiety disorders and substance abuse
What is the difference between delirium and dementia?
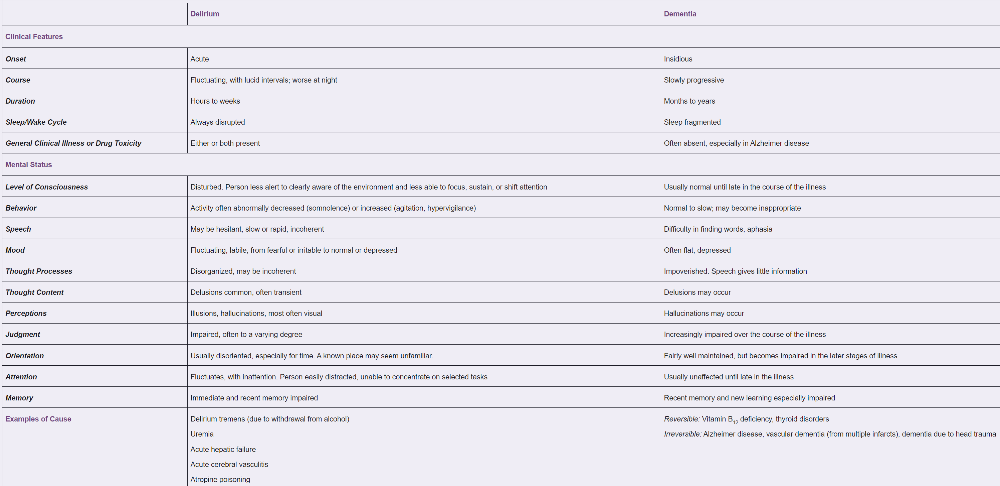
Delirium
- A multifactorial syndrome, is an acute confusional state
- Sudden onset
- Fluctuating course; inattention; and, at times, changing levels of consciousness
- Confusion Assessment Method screens at risk pts
Dementia
- characterized by a decline in at least two cognitive domains (e.g., loss of memory, attention, language, or visuospatial or executive functioning)
- Mini-Mental State Examination is the best-known screening test for dementia
What are components of the MMSE?
Why are they being assessed?
- orientation
- registration
- attention
- calculation
- recall
- language
Score of 25 or higher is normal
The Mini-Mental State Examination is the best-known screening test for dementia
What is Beers criteria?
What is the concern regarding anticholinergic medication in elderly?
Learn about drug–drug interactions and consult the 2019 AGS Beers Criteria, widely used by health care providers, educators, and policymakers. In addition to a list of hazardous drugs for older adults, this new criteria now include lists of select drugs that should be avoided or have their dose adjusted based on the individual’s kidney function and select drug–drug interactions documented to be associated with harms in older adults
How to palpate lymph nodes?
- Using the pads of your index and middle fingers
- Palpate gently in a gentle rotary motion, moving the skin over the underlying tissues in each area.
- Note lymph node size, shape, delimitation (discrete or matted together), mobility, consistency, and any tenderness.
- Small, mobile, discrete, nontender nodes, sometimes termed “shotty,” are frequently found in normal people.
- Describe enlarged nodes in two dimensions,
maximal length and width, for example, 1 cm × 2 cm.
- Tender nodes suggest inflammation
- Hard or fixed nodes (fixed to underlying structures and not movable on palpation) suggest malignancy.
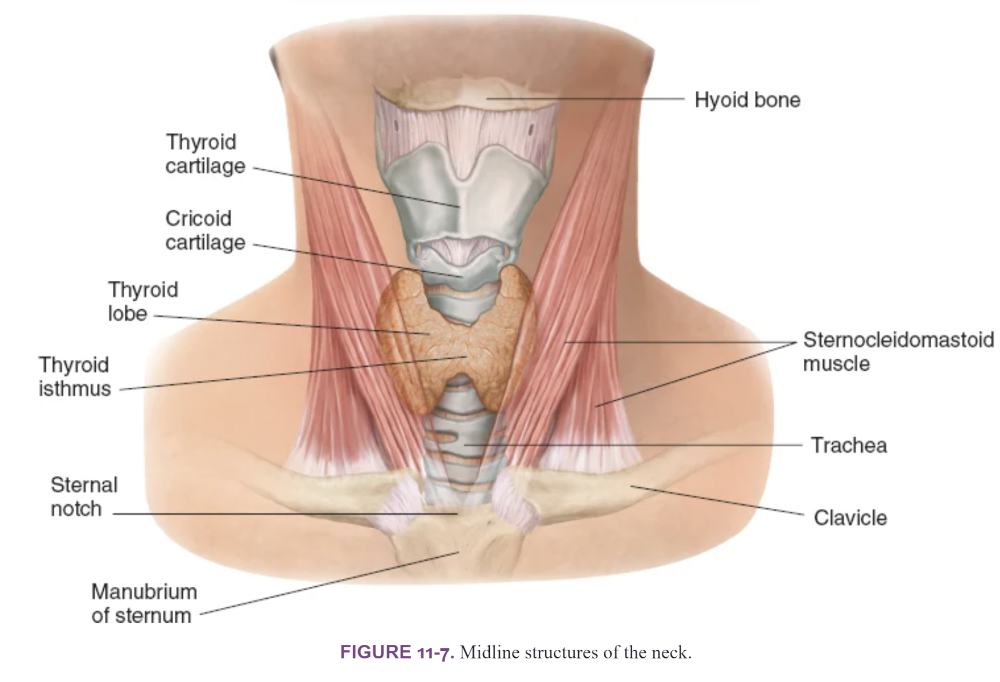
Recognize normal neck anatomy?
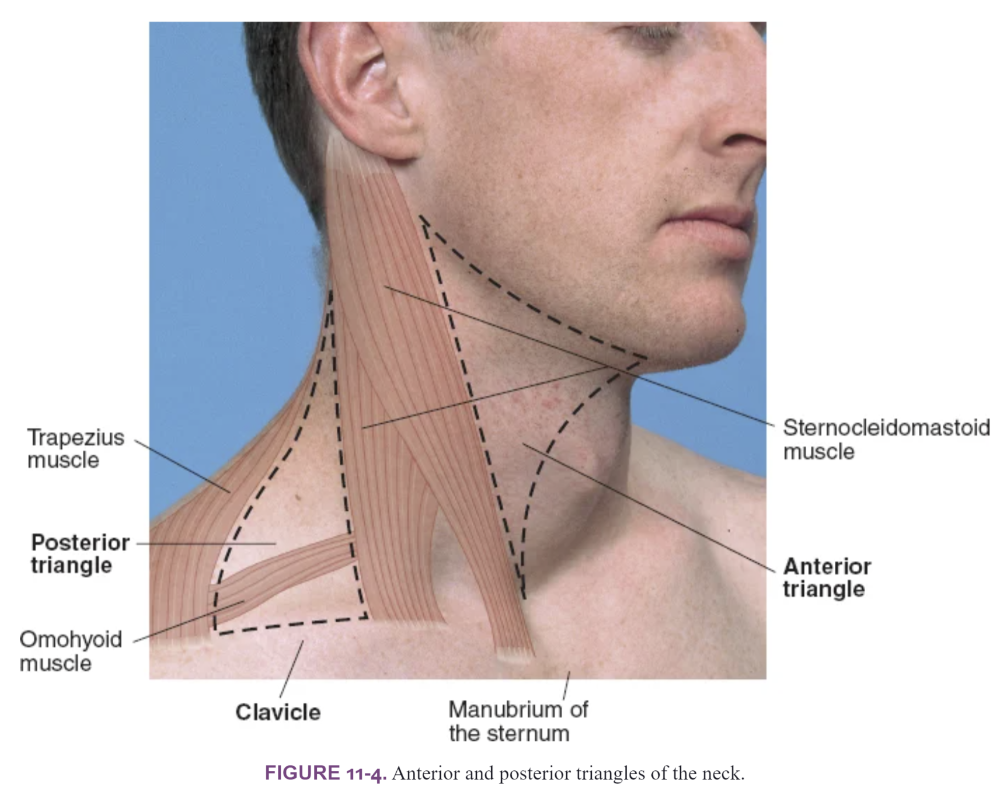
- Anterior cervical triangle: the mandible above, the SCM muscle laterally, and the midline of the neck medially.
- Posterior cervical triangle: the SCM muscle, the trapezius, and the clavicle. Note that a portion of the omohyoid muscle crosses the lower portion of this triangle and can be mistaken for a lymph node or mass.
- Thyroid gland is usually located above the suprasternal notch
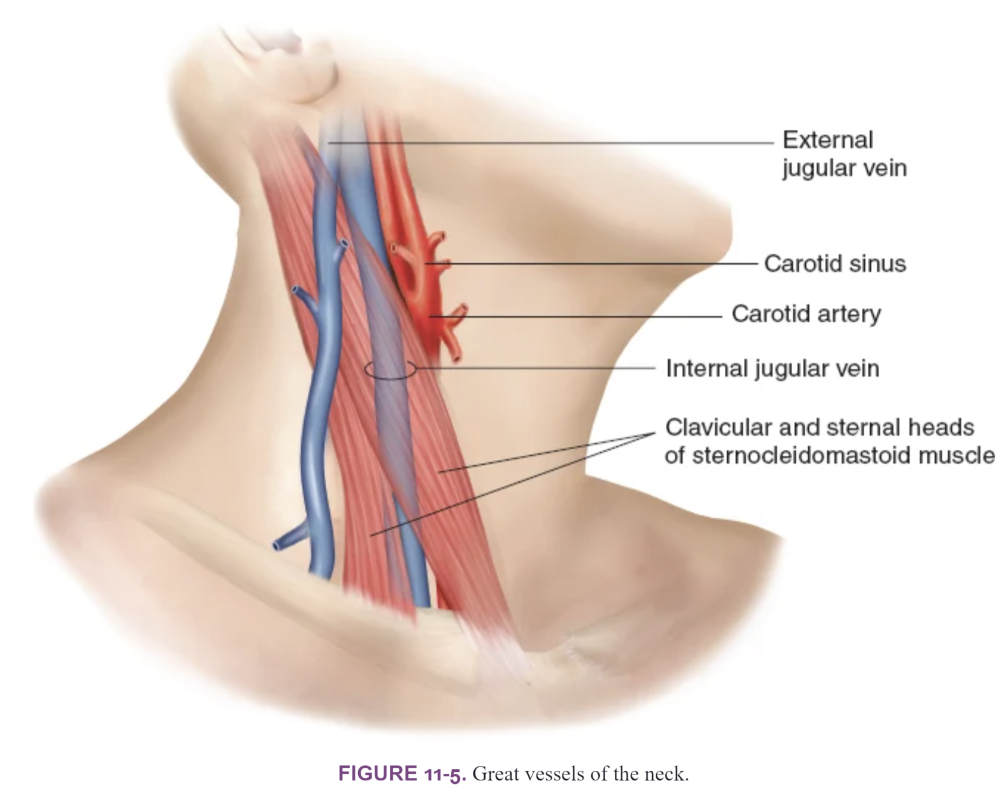
Great Vessels of the Neck
- SCM muscles run the great vessels of the neck: the carotid artery and the internal jugular vein
- The external jugular vein passes diagonally over the surface of the SCM muscle and may be helpful when trying to identify the jugular venous pressure
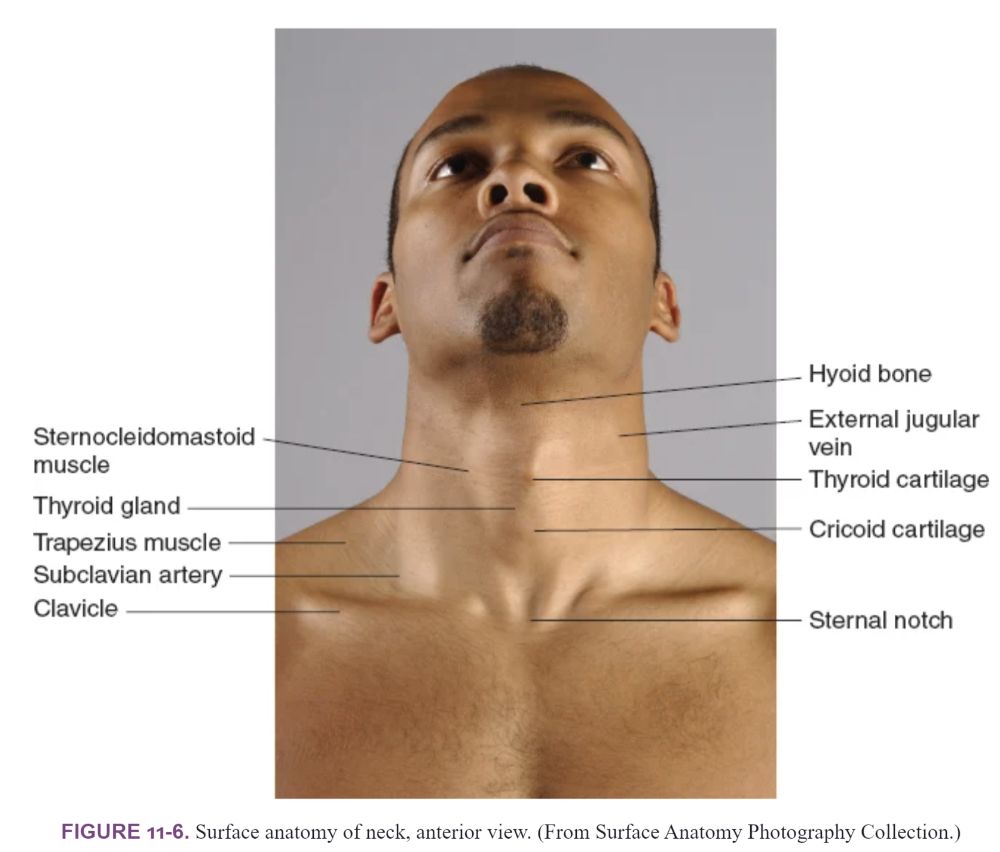
Midline structures of the neck
- (1) the mobile hyoid bone just below the mandible
- (2) the thyroid cartilage, readily identified by the notch on its superior edge
- (3) the cricoid cartilage
- (4) the tracheal rings
- (5) the thyroid gland
Midline structures of the neck
What is the best position for palpating the thyroid?
- Find your landmarks—the notched thyroid cartilage and the cricoid cartilage below it.
- Locate the thyroid isthmus, usually overlying the second, third, and fourth tracheal rings.
Posterior Approach
- Stand behind pt
- Ask the patient to flex the neck slightly forward to relax the SCM muscles.
- Gently place the fingers of both hands on the patient’s neck so that your index fingers are just below the cricoid cartilage
- Ask the patient to sip and swallow water as before.
- Feel for the thyroid isthmus rising up under your finger pads.
- Displace the trachea to the right with the fingers of the left hand; with the right-hand fingers, palpate laterally for the right lobe of the thyroid in the space between the displaced trachea and the relaxed SCM muscle
Anterior Approach
- Attempt to locate the thyroid isthmus by palpating between the cricoid cartilage and the suprasternal notch
- Use one hand to slightly retract the SCM muscle while using the other to palpate the thyroid
- Ask the patient to sip some water and to extend the neck again and swallow.
- Watch for upward movement of the thyroid gland, noting its contour and symmetry.
Thyroid gland is usually located above the suprasternal notch
Note the size, shape, and consistency (soft, firm, or hard) of the gland and identify any nodules or tenderness
- What is the proper technique when using the ophthalmoscope?
- Darken the room. Switch on the ophthalmoscope light and turn the lens disc until you see the large round beam of white light. Shine the light on the back of your hand to check the type of light, its desired brightness, and the electrical charge of the ophthalmoscope.
- Turn the focusing wheel to the 0 diopter. (A diopter is a unit that measures the power of a lens to converge or diverge light.) At this diopter, the lens neither converges nor diverges light. Keep your finger on the edge of the lens disc so that you can turn the focusing wheel to focus the lens when you examine the fundus.
- Hold the ophthalmoscope in your right hand and use your right eye to examine the patient’s right eye; hold it in your left hand and use your left eye to examine the patient’s left eye. This keeps you from bumping the patient’s nose and gives you more mobility and closer range for visualizing the fundus. With practice, you will become accustomed to using your nondominant eye.
- Hold the ophthalmoscope firmly braced against the medial aspect of your bony orbit, with the handle tilted laterally at about 20 degrees slant from the vertical. Check to make sure you can see clearly through the aperture. Instruct the patient to look slightly up and over your shoulder at a point directly ahead on the wall.
- Place yourself about 15 inches away from the patient and at an angle 15° lateral to the patient’s line of vision. Shine the light beam on the pupil and look for the orange glow in the pupil—the red reflex. Note any opacities interrupting the red reflex. If you are nearsighted and have taken off your glasses, you may need to adjust the focusing wheel toward the minus/red diopters until the structures you see at a distance is in focus.
- Now place the thumb of your other hand across the patient’s eyebrow, which steadies your examining hand. Keeping the light beam focused on the red reflex, move in with the ophthalmoscope on the 15-degree angle toward the pupil until you are very close to it, almost touching the patient’s eyelashes and the thumb of your other hand.
- Try to keep both eyes open and relaxed, as if gazing into the distance, to help minimize any fluctuating blurriness as your eyes attempt to accommodate.
- You may need to lower the brightness of the light beam to make the examination more comfortable for the patient, avoid hippus (spasm of the pupil), and improve your observations.
- What are the following test indicated for?
- Tonometry
- Snellen tests
- Fluorescein Staining
- Cover/uncover
- Red reflex
-
Tonometry
- test to measure the pressure inside your eyes
-
Snellen tests
- Test the acuity of central vision
- Position the patient 20 ft from the chart
- Ask to read the smallest line
-
Fluorescein Staining
- staining of the eye to detect corneal damage
- use the cobalt lamp
-
Cover/uncover
- Used to detect strabismus
- The child is asked to visually fix on a target at distance or near
- A cover is placed over one eye for a few seconds and then rapidly removed
- The eye that was under the cover is observed for movement
- Once it is uncovered, this eye must shift back into the straight-ahead position to re-fixate on the object if it became deviated while covered= strabismus
- Used to detect strabismus
-
Red reflex
- Screening test for cataracts
- Recognize Strabismus, Dacryostenosis, significance of eye turn in infants

Strabismus
- dysconjugate gaze
- Visual defect in which the eyes are
misaligned and point in different directions
- Non-paralytic or paralytic type
- Frequently present only when looking at near objects
- The number one cause of amblyopia (lazy eye) in children
- Caused by any disorder that interferes with vision or
with
visual pathways in the brain - Significant accommodation results in a reflexive ocular convergence, forcing one eye medially off alignment
- Appears in children from 6 months to seven years of age with an average age of onset at 2-3 years of age
- Risk factors: low birth weight/prematurity, + family hx
Dacryostenosis- blocked tear duct
- Usually presents within the first few weeks of life with persistent tearing, crusting of the lashes and mucopurulent discharge
- Tears spill over the lower lid and there is a persistent “wet look” in the involved eye (s)
- On exam, reflux of mucopurulent material from either punctum can be elicited by gently pressing over the nasolacrimal sac of the involved eye (s)
Eye Turn in infants
- Infantile strabismus (congenital strabismus)
Presents with profound esotropia before 6 months of age - Apparent by 3 months of age
- Refraction of each eye is normal
- Full ocular examination
- Ask if child has abnormal face or head position
- Ask parents to bring in un-posed photos of the child
- Test visual acuity using the tumbling E chart or Allen picture cards (start age 3-4 years)
What is Presbyopia?
- Aging vision
- Found in middle-aged and older adults
- Causes focusing problems for near vision
- See better when the card is farther away
What are the symptons of macular degeneration?
- Sudden visual loss is unilateral and painless
- Slow central vision loss in older
adults
- gradual vision loss
- Drusen are yellowish round spots that vary from tiny to small around the posterior pole between the optic disc & macula
****think of the doctor from Virign River show***
What is clinical presentation of subconjunctival hemorrhage?
- RED PAINLESS EYE
- Sudden onset of bright red blood
- No vision loss or pain
- Unilateral: may have just had coughing, sneezing, straining
Be able to differentiate between the presentation of chalazion, hordeolum, blepharitis
What is Chalazion?
What is Hordeolum?
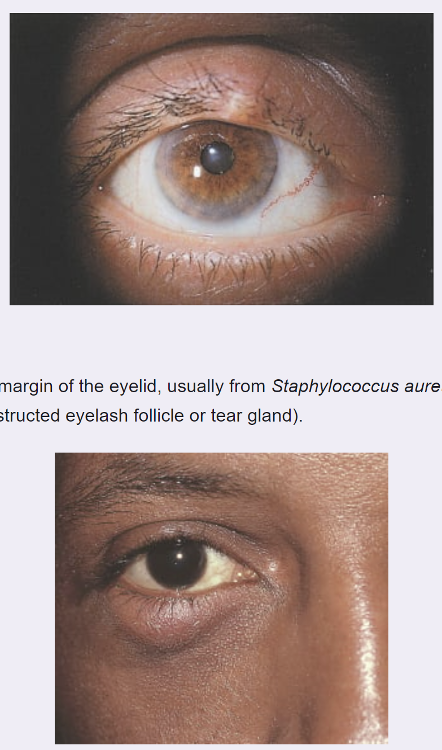
Hordeolum- Stye
- PAINFUL, TENDER, RED infection at the inner or outer margin of the eyelid
-
Caused by
Staphylococcus aureus
- Inner margin can be from an obstructed meibomian gland
- Outer margin can be from an obstructed eyelash follicle or tear gland
Chalazion
- A subacute NONTENDER, usually painless nodule caused by a blocked meibomian gland
- May become acutely inflamed
- Points inside the lid rather than on the lid margin
What is presentation of blepharitis?
Blepharitis
- A chronic inflammation of the eyelids at the base of the hair follicles
- Often caused by S. aureus.
- There is also a scaling seborrheic variant
Typical complaints are:
- Scaling and inflammation of eyelid margins
- Crusting and tearing around the eyes (especially upon awakening)
- Itching and burning of the eyes
- Red eyes
- Gritty sensation in eyes
- Some cases may be asymptomatic and identified on routine examination
On examination, may see the following:
- Eyelid margins erythematous with yellowish,
oily
scales - Lashes often matted with debris within the lashes
- Conjunctival infection or mild mucus discharge
may
also be present
What is the clinical presentation of:
Acute Bacterial conjunctivitis?
Bacterial
- Acute onset of burning
- Irritation
-
Tearing
and a mucopurulent or purulent discharge
- Patients usually report that their eyelids are matted together on awakening
- VISION NOT AFFECTED
-
On examination:
- conjunctival swelling and mild eyelid edema
- Usually self-limited and does not cause serious harm
- Infection usually begins in one eye and then becomes bilateral in 2-5 days
-
Most common microbes:
- Staphylococcus aureus (most common pathogen in adults)
- Streptococcus pneumonia (Most common cause in children)
- Haemophilus influenza (More common in children)
- HIGHLY CONTAGIOUS
- Spread by direct contact
with the patient secretions or with contaminated objects and
surfaces
- hands, towels
- Cultures should be obtained in patients who have severe inflammation (hyperacute purulent conjunctivitis) or chronic, recurrent conjunctivitis and in patients who do not respond to treatment
What is the clinical presentation of:
Viral conjunctivitis?
- Acutely red eye
- Watery discharge
- Conjunctival swelling
- Tender preauricular node
- In some cases: photophobia and a foreign body sensation (gritty, burning sensation)
- VIRAL AFFECTS BOTH
EYES
- May be affected simultaneously, or the second eye may become involved a few days after the first eye
- History of recent URI common
- Self-limited and rarely results in serious harm
- Herpes simplex conjunctivitis may be accompanied by fever
blister on the lip or face and occurs most frequently in
immunosuppressed persons
- In newborns evaluate parent’s
sexual history, mothers prenatal care and timing of onset
of
symptoms from birth
- In newborns evaluate parent’s
sexual history, mothers prenatal care and timing of onset
of
- Viruses: Adenovirus/Herpes
What is the clinical presentation of:
Allergic conjunctivitis?
- Presents with
- Intermittent bouts of bilateral itching
- Tearing
- Redness and mild eyelid swelling
- On exam
- Palpebral conjunctiva may have a cobblestone appearance
- Personal and/or family history is often positive for other allergic conditions such as allergic rhinitis, asthma and eczema
What is the evaluation of conjunctivitis
- Thorough ocular, medical, sexual and medication history
- Determine if symptoms are unilateral or bilateral, acute, hyperacute or chronic, or intermittent
- In newborns evaluate parent’s sexual history, mothers prenatal care and timing of onset of symptoms from birth
- Full eye exam, visual testing and examination of regional lymph nodes
- Diagnostic tests
- Cultures usually are not required in patients with mild conjunctivitis of suspected bacterial, viral or allergic origin
- Cultures should be obtained in patients who have severe inflammation (hyperacute purulent conjunctivitis) or chronic, recurrent conjunctivitis and in patients who do not respond to treatment
- In
conjunctivitis:
- Redness of the conjunctiva is diffuse, pain is minimal
- There is no visual loss
- Pupil size and reactivity are normal
What are RED FLAGS: Indicating serious eye issues
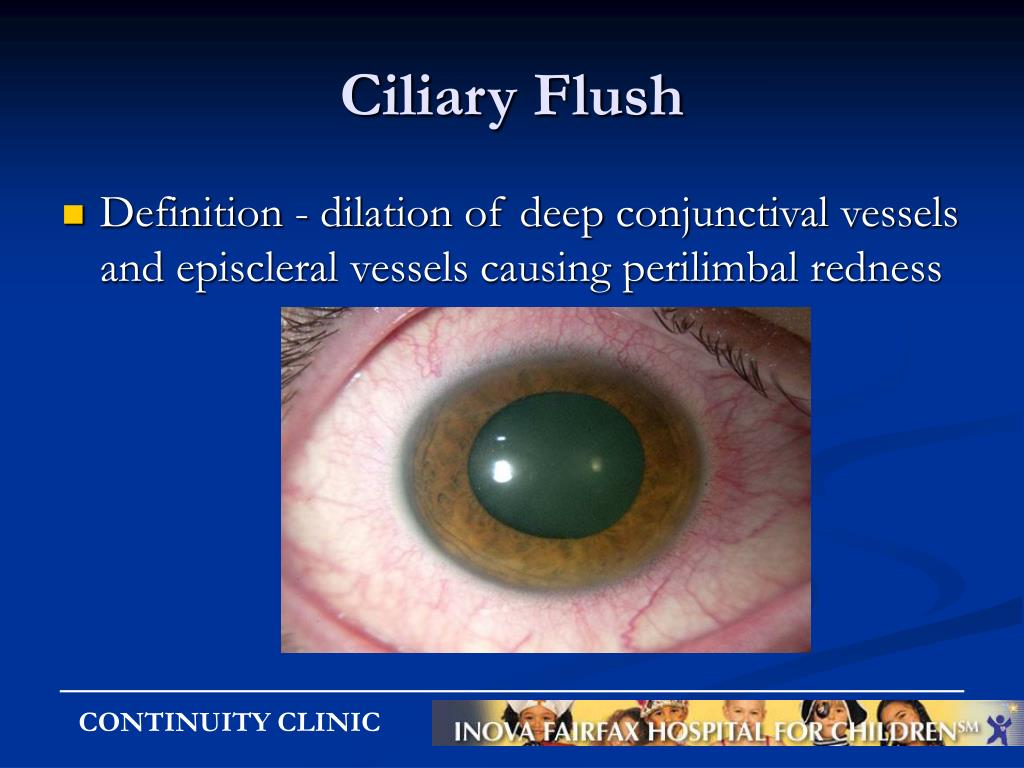
Important to distinguish conjunctivitis from other more serious conditions causing red eye (iritis, keratitis, acute angle closure glaucoma, foreign body).
In conjunctivitis:
- Redness of the conjunctiva is diffuse, pain is minimal
- There is no visual loss
- Pupil size and reactivity are normal
Red flag or warning signs that indicate a more serious ophthalmic
problem than
conjunctivitis
- Reduction of visual acuity
- Ciliary flush: A pattern of injection in which the redness is most pronounced in a ring at the limbus (the limbus is the transition zone between the cornea and the sclera)
- Photophobia
- Severe foreign body sensation that prevents the patient from keeping the eye open
- Corneal opacity
- Fixed pupil
- Severe headache with nausea
What is papilledema and what does it signify?
- Swelling of the optic disc and anterior bulging of the physiologic cup= increased pressure causes optic nerve head swelling associated with increased intracranial pressure
- Color pink, hyperemic
- Often with loss of venous pulsations
- Disc vessels more visible, more numerous, curve over the borders of the disc
- Disc swollen with margins blurred
- The physiologic cup is not visible
-
What does it signify?
- Signals serious disorders of the brain, such as meningitis, subarachnoid hemorrhage, trauma, and intracranial mass, lesions
What are eye findings in Thyroid disease?
- Abnormal protrusion or proptosis
- Lagophthalmos, or failure of the eyelids to close in thyroid dx
- Exophthalmos or increased axial projection thyroid dx
HypoT
- Scaliness occurs in seborrheic dermatitis, lateral sparseness in hypothyroidism
HyperT
- With Graves disease, eye signs such as stare, lid lag, and exophthalmos
- Lid lag of hyperthyroidism, a rim of sclera is visible above the iris with downward gaze
- Proptosis, an abnormal protrusion of the eyeballs in
hyperthyroidism
- characteristic stare
Eye findings for hyperlipidemia disorders
What are findings that indicate hyperlipemia?
Xanthelasma
- Slightly raised, yellowish, well-circumscribed cholesterol-filled plaques that appear along the nasal portions of one or both eyelids
Presentation of a pterygium
What are clinical findings of pterygium?
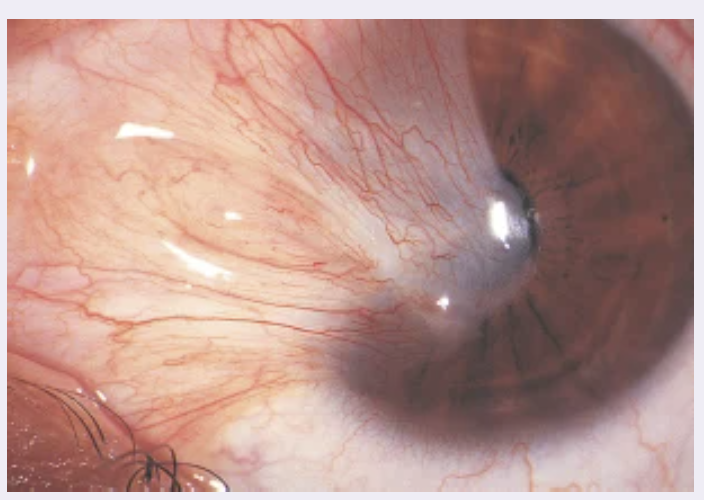
- A
triangular
thickening of the bulbar conjunctiva (yellow wedge-shaped
thickening of conjunctiva)
- grows slowly across the outer surface of the cornea, usually from the nasal side.
- Reddening and irritation may occur.
- May interfere with vision as it encroaches on the pupil.
- Caused by UV damage
- Treatment: wear sun-glasses, refer for surgery if affecting vision
Presentation of presentation of a pinguecula
What are clinical findings of pinguecula?
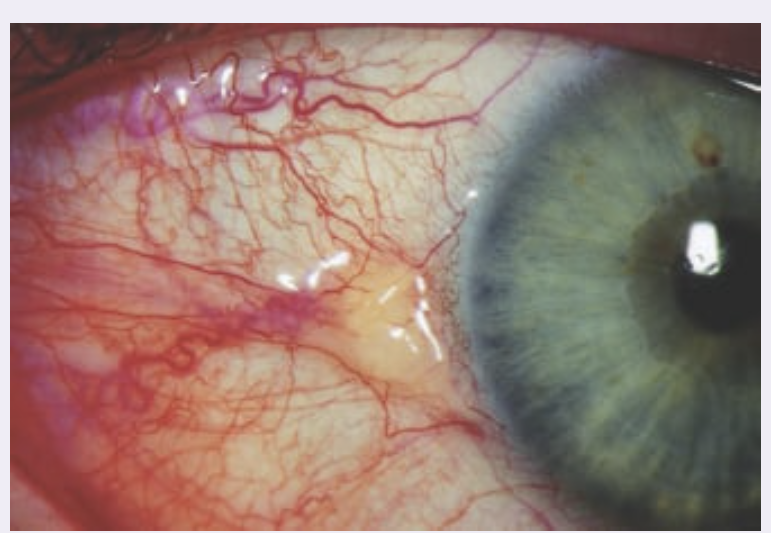
- Harmless yellowish triangular nodule in the bulbar conjunctiva on either side of the iris.
- Appears frequently with aging, first on the nasal and then on the temporal side.
- Cause UV damage
What are normal findings when checking for PERRLA
Pupils Equal, Round, Reactive to Light and Accommodation
- Note if the pupils are large (>5 mm), small (<3 mm), or unequal
- The direct reaction (pupillary constriction in the
same eye)
The consensual reaction (pupillary constriction in the opposite eye)
What are clinical presentations of otitis externa?
- an inflammation or infection of the ear canal
- Ear pain that presents gradually or sudden
- Sensation of fullness or obstruction in the ear ** think of ear wax buildup
- Canal erythematous and edematous
- Purulent discharge
- Conductive hearing loss may occur
-
Itching
may occur and is the predominant
symptom with fungal infections - Uncommon to see fever
Predisposing factors
- Frequent exposure to moisture (swimming,
humid, warm climates) - Aggressive cleaning of the canal or trauma
- Allergies or skin conditions such as psoriasis
- Wearing
hearing aids, earplugs on regular
basis
Common pathogens
- Pseudomonas (most common)
- Staphylococci epidermis
- Staphylococci aureus
- Fungal (about 9% of the cases)
What is the presentation of otitis media with effusion?
- Accumulation of serous fluid in the middle ear without signs of infection
- CLINICAL SIGNS of acute infection ARE ABSENT
-
When patients are symptomatic, the predominant symptom
is hearing loss
- Other nonspecific symptoms that may occur in children with OME include:
- Ear pain
- Sleep disturbance
- A feeling of fullness in the ear *** because it is full of fluid
- Tinnitus
- Often occurs after acute otitis media (AOM), but it also may occur with eustachian tube obstruction in the absence of AOM
- Most frequent cause of air conduction hearing loss in school age children
- Affects 80% of children by four years of age
- Can occur in adults but more frequent in children
Otoscopic findings
- Tympanic membrane in a neutral or retracted position
- Color of TM varies from gray to translucent
- Fluid behind TM may be amber colored or clear
- Impaired mobility of the tympanic membrane when positive pressure is applied with the bulb during pneumatic otoscopy
- An air-fluid level may be present behind the tympanic membrane
- Audiogram may show a 15-30 dB air conduction loss with normal bone conduction
What is otitis media?
What are clinical presentations of otitis media infection?
- Infection in the middle ear
- Commonly follows a viral URI
- URI symptoms
- Ear pain
- Otorrhea- ear drainage
- Fever
- Hearing loss and or vertigo
- Diarrhea, nausea and vomiting are common in children
- Irritability (especially in children)
- Evaluation:
- Hx of symptoms, onset and recent sick
contacts and other risk factors
- Hx of symptoms, onset and recent sick
- PE to include assessment
of :
- Eyes, ears, pharynx, teeth, sinus
tenderness,
nose, lymph nodes and chest
- Eyes, ears, pharynx, teeth, sinus
tenderness,
- Diagnosis is based on acute history and the
appearance of the tympanic membrane:- Full or bulging TM
- Marked erythema
- Distorted light reflex
- Absent or obscured landmarks
- Decreased or absent mobility of TM by pneumatic otoscopy
What is Cholesteatoma presentation?
Middle ear disorders
Abnormal collection of skin cells deep inside your ear
Complication of AOM
What is Epistaxis?
Common causes and management?
- Bleeding from the nasal passages
- originate in the paranasal sinuses or nasopharynx
- Causes:
- Trauma (especially nose-picking)
- Tumors
- Foreign Bodies
- Inflammation- allergic rhinitis
- Drying and crusting of the nasal mucosa- low humidity, dry air
- Chronic excoriation chronic intranasal drug use- cocaine/steroid spray
- Anticoagulants, NSAIDs, vascular malformations, and coagulopathies
- Management
- Clinician sprays the nares with
oxymetazoline
(Afrin, if avail) - Patient pinches
the anterior nasal septum (not
the bridge of the nose) while head is tilted
forward; continue pressure for 10-15 minutes
(may also apply ice over the nose) - If bleeding continues, may need to
cauterize
with sliver nitrate stick and if needed packing
and possible balloon catheters
- Clinician sprays the nares with
oxymetazoline
What is rhinitis medicamentosa?
How do you avoid it?
- Drug-induced rhinitis occurs with excessive use of topical decongestants
- Inquire about all medications or drugs
What is the Weber test ?
How and why do you perform it?
- Test for lateralization
How to perform the test:
- Set the fork into light vibration by briskly stroking the prongs (the “U”) between the thumb and index finger or by tapping the prongs on your forearm just in front of your elbow.
- Place the base of the lightly vibrating tuning fork firmly on top of the patient’s head or on the midforehead
- Ask where the patient hears the sound best: “On one side or both sides?”
Results
- Unilateral conductive hearing loss, sound is heard in the impaired ear
- Unilateral sensorineural hearing loss, sound is heard in the good ear
What is the Rinne Test?
How and Why do you perform it?
Compare air conduction (AC) and bone conduction (BC)
How do you perform it?
- Place the base of a lightly vibrating tuning fork on the mastoid bone, behind the ear and level with the canal
- When the patient can no longer hear the sound, quickly place the prongs of the fork close to the ear canal and ask if the patient hears a vibration
Results
- Sound is NORMALLY heard longer in air then in bone
- In conductive hearing loss, sound is heard through bone longer than it is through air (BC = AC or BC > AC).
- In sensorineural hearing loss, sound is heard longer through air (AC > BC).
Difference in Conductive and Sensorineural loss?
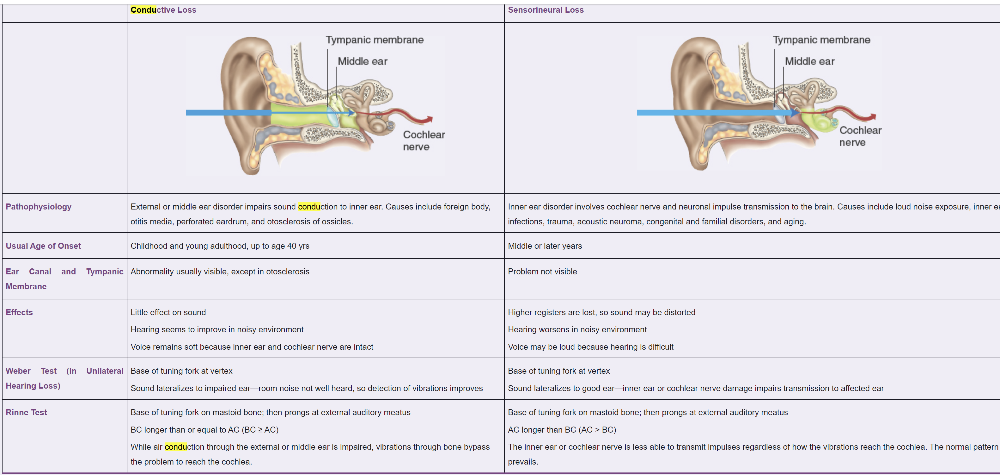
- The first part of the hearing pathway, from the external ear
through the middle ear, is known as the conductive phase.
- Hearing disorders of the external and middle ear cause conductive hearing loss.
- The second part of
the pathway, involving the cochlea and the cochlear branch of CN
VIII, is the sensorineural phase
- Disorders of the inner ear cause sensorineural hearing loss
- Air conduction (AC) describes the normal first phase in the hearing pathway, where sound waves travel through the air and are transmitted from the external and middle ear to the cochlea.
- An alternative pathway, known as bone conduction (BC), bypasses the external and middle ear and is used for testing purposes.
- A vibrating tuning fork, placed on the head, sets the bone of
the skull into vibration and stimulates the cochlea directly.
- In those with normal hearing, air conduction is more sensitive than bone conduction (AC > BC).
Presentation of acute bacterial sinusitus
- Onset with persistent s/sx compatible
with acute rhinosinusitis, lasting for
>10 days without any evidence of
clinical improvement OR - Onset with severe symptoms
or signs
of high fever (>102°F) and purulent
nasal discharge or facial pain lasting
for at least 3–4 consecutive days at
the beginning of illness, OR - Onset with
worsening symptoms or
signs characterized by the new onset
of fever, headache, or increase in
nasal discharge following a typical
viral URI that lasted 5–6 days and was
initially improving
Objective signs include:
- Edematous and hyperemic nasal mucosa
- Narrowing of the middle meatus
- Inferior turbinate hypertrophy
- Palpated tenderness over affected sinus (rare
in young children) - Pain over affected sinus when patient
bends
forward - Purulent nasal discharge or copious rhinorrhea
- Periorbital swelling may be seen in
ethmoid
sinusitis
Expected lab findings in mononucleosis?
Labs: Elevated LFTs, lymphocytosis
What is clinical presentation of viral pharyngitis?
- Typical
gradual onset of:
- Pharyngeal pain and dysphagia
- Erythema/inflammation of pharynx and tonsils and possible exudates
- Fever
- Rhinorrhea
- Cough
- Hoarseness
What is clinical presentation of strep throat?
-
Acute
Onset of the following:
- Pharyngeal pain and dysphagia
- Fever
- Headache and malaise
- Tender and enlarged anterior cervical nodes
- Purulent exudates on tonsils
- Tonsils and pharynx intensely erythematous
- Petechia on soft palate
What are guideline recommendations for oral health?
- Use of fluoride-containing toothpastes reduces tooth decay, and brushing and flossing retard periodontal disease by removing bacterial plaques.
- Urge patients to seek dental care at least annually to receive the benefits of more specialized preventive care such as scaling, planing of roots, and topical fluorides.
- Address diet and tobacco use.
- As with children, adults should avoid excessive intake of foods high in starches and refined sugars such as sucrose, which enhance attachment and colonization of cariogenic bacteria.
- Urge patients to avoid use of all tobacco products and to limit alcohol consumption to reduce risk of oral cancer.
- Saliva cleanses and lubricates the mouth. Many medications reduce salivary flow, increasing risk for tooth decay, mucositis, and gum disease from xerostomia, especially for older adults. If medications cannot be changed, recommend drinking higher amounts of water and chewing sugarless gum.
- For those wearing dentures, recommend
removal and cleaning each night to reduce bacterial plaque and risk
of malodor.
- Regular massage of the gums relieves soreness and pressure from dentures on the underlying soft tissue.