Instructions for Side by Side Printing
- Print the notecards
- Fold each page in half along the solid vertical line
- Cut out the notecards by cutting along each horizontal dotted line
- Optional: Glue, tape or staple the ends of each notecard together
mastering A&P chapter 24
front 1 What is the difference between anabolism and catabolism? | back 1 Anabolism uses raw material to synthesize essential compounds and catabolism decomposes substances to provide energy cells need to function. |
front 2 2. What two essential ingredients are required in catabolic reaction? | back 2 2. Oxygen and broken down organic molecules |
front 3 What are organic molecules broken down by? | back 3 Intracellular enzymes |
front 4 What are two other names for the digestive tract? | back 4 Gastrointestinal tract (GI) and alimentary canal |
front 5 What is the distance of the digestive tract? What all does it pass through? | back 5 Oral cavity to anus; pharynx, esophagus, stomach, and small and large intestines |
front 6 What are the six functions of the digestive system? | back 6 Ingestion, mechanical processing, digestion, secretion, absorption, and excretion |
front 7 What is ingestion? When does it occur? | back 7 Bringing food in; when materials enter Digestive tract |
front 8 What is mechanical processing? | back 8 The crushing and shearing |
front 9 Where does digestion occur? What is it? | back 9 Stomach; chemical breakdown of food for absorption |
front 10 What is secretion? How are thing secreted in the digestive tract? | back 10 Release of water, acids, enzymes, buffers, and salts; by epithelium and glandular organs |
front 11 What occurs in absorption? | back 11 Organic substances move |
front 12 What occurs in excretion? | back 12 Materials are removed |
front 13 What do visceral smooth muscle cells rely on? Why? | back 13 Self-communication; lack direct connection with motor neuron |
front 14 How are visceral smooth muscle cells arranged? How are they connected? | back 14 Sheets or layers; electronically by gap junction and mechanically by dense bodies |
front 15 What kind of stimulation can visceral smooth muscle cells have? How are some stimulated? | back 15 Neural, hormonal, or chemical; pacesetter cells |
front 16 Where are some visceral smooth muscle cells located? | back 16 Digestive tract walls, gallbladder, bladder, etc. |
front 17 What does the plasticity of smooth muscle important for? | back 17 Allows organs to adapt shape and still contract |
front 18 What is smooth muscle tone? | back 18 Normal background activity and tension due to various stimulations |
front 19 What are the two types of movement and regulations of the digestive tract? | back 19 Peristalsis and segmentation |
front 20 What is peristalsis? | back 20 Wave of muscle contraction that propel bolus through digestive tract |
front 21 What is segmentation? Where does it occur? | back 21 Cycles of contraction that churn & fragment bolus; In many areas of small intestine & some of large |
front 22 What is the primary stimulus for digestive activity? | back 22 Local factors |
front 23 What are the short reflexes of neurons controlled by? | back 23 Myenteric plexus |
front 24 What are long reflexes of neurons controlled by? | back 24 Interneurons and motor neurons |
front 25 What are the primary stimulus types for digestive activities? | back 25 pH of lumen; physical distortion of DT wall, and presence of chemicals |
front 26 What kinds of hormones control the digestive tract and where are they produced? | back 26 Peptides; enteroendocrine cells within epithelium |
front 27 What are mesenteries? What two things do they do? | back 27 Double sheet of peritoneal membrane; provides access route for blood vessels, nerves, and lymphatic vessels- also stabilizes position of attached digestive organs |
front 28 What does the peritoneal cavity do? | back 28 Encloses stomach and most of the intestines |
front 29 What is the peritoneal cavity lined with? What are the parts of it? What does it secrete and why? | back 29 Serous peritoneum; parietal and visceral; peritoneal fluid to lubricate organs |
front 30 What are the two mesenteries that exist during development? | back 30 Dorsal and ventral |
front 31 What does the dorsal become? | back 31 Greater omentum, mesentery proper, & mesocolon |
front 32 What does the ventral become? | back 32 Lesser omentum and falciform ligament |
front 33 Which is more efficient in propelling intestinal content from one place to another: peristalsis or segmentation? | back 33 Peristalsis |
front 34 What effect would a drug that blocks parasympathetic stimulation of the digestive tract have on peristalsis? | back 34 It would slow it down because the muscle tone would be increased |
front 35 where does the majority of digestion happen? | back 35 stomach |
front 36 what materials are found in the stomach? what do they create? | back 36 food, saliva, and gastric gland secretions; chyme |
front 37 what are the regions found in the stomach? | back 37 fundus, cardia, body, and pylorus |
front 38 where is the fundus found? | back 38 superior to esophageal connection |
front 39 what does the cardia do and why? | back 39 secrete mucus to protect esophagus from acid/enzymes |
front 40 what is the largest portion of the stomach? | back 40 body |
front 41 what leads to the small intestine in the stomach? | back 41 pylorus |
front 42 where is the lesser curvature found? | back 42 medal surface |
front 43 where is the greater curvature found? | back 43 lateral and inferior surfaces |
front 44 what is found in addition to circular and longitudinal layers in muscularis externa? | back 44 oblique muscle layer |
front 45 what are rugae and what do they allow? | back 45 mucosal wrinkles that flatten when stomach fills; they allow muscles to expand |
front 46 what are the pyloric structures? | back 46 pyloric antrum, pyloric canal, and pyloric sphincter |
front 47 what portion of the pylorus is a smooth muscle band that regulates release of chyme into duodenum? | back 47 pyloric sphincter |
front 48 what portion of the pylorus is empties into small intestine? | back 48 pyloric canal |
front 49 what portion of the pylorus is connected the stomach body? | back 49 pyloric antrum |
front 50 what do gastric glands secrete? where do gastic glands open? what do the stem cell at the neck do? | back 50 most of the acid and enzymes enabling gastric digestion; to stomach luman through gastric pits; replace cells lost into chyme |
front 51 what do parietal cells secrete? what are these secretions used for? | back 51 intrinsic factor- B12 absorption; HCl- activates pepsinogen to keep stomach at pH~2 |
front 52 what do chief cells secrete? what does this secretion do? | back 52 pesinogen; becomes pepsin when activated |
front 53 what is pepsin? | back 53 active proteolytic enzyme |
front 54 what tow things are also secreted in infant? why? | back 54 rennin and gastric lipase to aid in digestion of milk |
front 55 what are G cells? what do they produce? | back 55 enteroendocrine cells; variety of hormones |
front 56 how is HCl produced? | back 56 carbonic anhydrace is sued to create bicarbonate ions and hydrogen ions from CO2 and H2O |
front 57 where is hydrogen released in HCl production? what else is released here? | back 57 into gastric gland lumen; chloride |
front 58 what happens to the bicarbonate? what is formed? | back 58 transported into blood; alkaline tide |
front 59 what can production of acid and enzymes by the gastric mucosea be controlled/regulated by? | back 59 controlled by CNS regulated by short reflexes of ENS and hormones of digestive tract |
front 60 what are the three phases of gastric control? | back 60 cephalic, gastric, and intestinal |
front 61 what do many intestinal structures do? | back 61 add surface area to increase aborption |
front 62 what are permanent transverse folds found mostly in the jejunum called? | back 62 plicae curcularis |
front 63 what are cell membreane extensions on simple columnar cell linings of villi surfaces called? | back 63 microvilli |
front 64 what are fingerlike projections on the mucosa called? | back 64 intestinal villi |
front 65 what do these three things do together? | back 65 add 600 times more area for absorption compared to smooth, flat walls |
front 66 where does 90% of absorption occur? where does the other 10% occur? | back 66 small intestine; large intestine |
front 67 what are the three regions of the intestine? | back 67 duodenum, jejunum, and IIeum |
front 68 describe the duodenum. | back 68 receives chyme from the stomach and digestive secretions from the liver, gallbladder and pancreas; mostly retroperitoneal; few pilcae circulari and small vili; many duodenal glands secreting mucus |
front 69 what I the duodenum's main function? | back 69 neutralizes acidic chyme |
front 70 describe and give the location of the jujunum. what happens here? | back 70 has numerous pilicae circularis and abundant, long vili; majority of chemical digestion and nutrient absorption |
front 71 why does the IIeum have few pilicae curculare and stumpy vili? | back 71 not much absorption occurs here. |
front 72 what does the iieum's submucosa contain? what does the iieum control? | back 72 aggregated lymphoid modules; material clow into cecum of large intestine |
front 73 which four of the five major hormones that regulate digestive activities are produced by the duodenum? | back 73 gastrin, secretin, gastric inhibitory peptide,and cholecystokinin |
front 74 are equal amounts of the hormones secreted every meal? | back 74 no only the amount needed of each is used |
front 75 what is gastrin secreted by? where is this located? | back 75 secreted by G cells in the pyloric antrium and enteroendocrine cells of the duodenum |
front 76 what stimulates gastrin particularly? what does it do? | back 76 food in the stomach and duodenum with high protein content; increases stomach mobility and production of gastric acids and enzymes |
front 77 when is secretin released from the duodenum? what does it do? | back 77 when chyme arrives; increases secretion of bile from liver and buffers from pancreas. also decreases gastric motility and secretory rates. (neutralizes pH also) |
front 78 which hormone is released by the duodenum when fats and carbohydrates enter the small intestine and inhibits gastric activity while increasing insulin release? what are secondary effects of this hormone? | back 78 gastric inhibitory peptide (GIP); stimulating duodenal glands, stimulating lipid synthesis in adipose, and increased skeletal muscle use |
front 79 which hormone is released by the duodenum are secrete when chyme arrives especially when it is high in lipids and partially digested proteins? what does this hormone do? | back 79 cholecystokinin; increase enzyme production and secretion from pancreas and bile from gallbladder. also inhibits gastric activity and may reduce hunger sensation is CNS |
front 80 regulation of gastric activity image | back 80  |
front 81 what are thew two central gastric reflexes? what are they under control by? | back 81 gastroenteric reflex and gastroileal reflex; under autonomic control |
front 82 which gastric reflex increases motility secretion? | back 82 gastroenteric reflex |
front 83 which gastric reflex triggers opening of ileocecal valve allowing passage of materials from small to large intestine? | back 83 gastroileal reflux |
front 84 what are the major functions of the large intestine during peristalsis? | back 84 1. reabsorption of water and compaction of content into feces. 2. absorption of inportant vitimins liberated by bacterial action and 3. storage of feces prior to defication |
front 85 what arethe three segments of the large intestine? | back 85 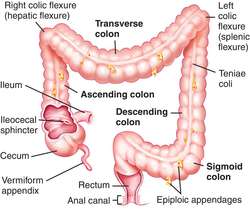 cecum, colon, and rectum |
front 86 what does the cecum begin? what does it contain and what is attached to it? | back 86 compaction; contains ileocecal valve and has an appendix attached. |
front 87 what does the appendix contain? what is the inflammation of the appendix called? | back 87 numerous lymphoid nodules; appendicitis |
front 88 what are the four parts of the colon? | back 88 ascending, transverse, descending, and sigmoid |
front 89 why is the rectum expandable? what triggers defecation urge? | back 89 for feces storage; fecal material within rectum |
front 90 what are large intestine characteristics associated with fecal production? | back 90 diameter is larger and wall is thinner that small intestines, lack of villi, abundance of mucous cells, many intestinal glands dominated by mucous glands; and no digestive enzymes produced |
front 91 what does mucus do in the large intestine? | back 91 provides lubercation for drier ad more compact fecal matter |
front 92 which anal sphincter is voluntary? which is involuntary? | back 92 external; iternal |
front 93 what two positive feedback loops are involved in defecation reflexes? | back 93 long and short |
front 94 which reflex is coordinated by the sacral parasympathetic system and stimulates mass movement into feces? | back 94 long reflex |
front 95 what is the other reflex responsible for? | back 95 stimulation of myeneric plexus to move feces in sigmoid colon and rectum |
front 96 what are the major accessory digestive organs and what do they do? | back 96 *salivary glands-produce saliva with mucins and enzymes
|
front 97 what is the larges visceral organ? | back 97 liver |
front 98 how many lobes does the liver have and what are they? | back 98 4- left, right,caudate, and quadrate |
front 99 what separates the left and right lobe ? what surrounds bare area? what marks fecal umbilical vein path? | back 99 falciform ligament; coronary ligament extension; round ligament |
front 100 what separates left lobe and caudate lobe? | back 100 inferior vena cava |
front 101 where is the quadrate lobe? | back 101 between the left lobe and gallbladder |
front 102 what are the structures associated with the liver | back 102  gallbladder, common bile duct, and porta hepatis |
front 103 what does the gallbladder do in association with the liver? | back 103 stores bile it produces temporarily |
front 104 what does the common bile duct do? | back 104 carries bile from the liver and gallbladder to duodenum |
front 105 what does the porta hepatis' function? | back 105 entry point for blood vessels and other structures from lesser omentum |
front 106 what are the lobules of the liver separated by? | back 106 interlobular septa |
front 107 what is in the corner of each lobule | back 107 a portal area or triad |
front 108 what makes up the portal area? | back 108 branch of portal vein, branch of hepatic artery, and branch of bile duct |
front 109 what ate the liver lobules composed of? | back 109 hepatocytes (liver cells) |
front 110 what are liver sinusoids? where do they drain? | back 110 blood vessel with nutrients and solutes and are regulated by hepatocytes central vein |
front 111 what else is found within the liver lobules? | back 111 phagocytic kupffer cells |
front 112 give the steps of bile movement in the liver after it is secreted. | back 112 secreted bile drains into bile canaliculi then bile ductules then bile ducts of the portal triad |
front 113 what is an effect if alcoholism and hepatitis? | back 113 degenerative changes in liver and constriction of blood supply |
front 114 what can increased pressure die to clot or damage create? what are some things this may lead to? | back 114 portal hypertension; vessel distension and rupture or ascities due to serous fluid leakage |
front 115 what are the three regions of the gallbladder? | back 115 fundus, body and neck |
front 116 where does the gallbladder drain fluid? | back 116 cystic duct |
front 117 what does the cystic duct merge with and what does it create | back 117 right and left common hepatic duct of liver to become common bile duct |
front 118 besides storing bile, what else does the gallbladder do? | back 118 concentrate it |
front 119 when and where is the bile released? what hormone controls it? | back 119 at mealtime into duodenum when hepatopancreatic sphinter is relaxed; CCK |
front 120 what doe bile salts do? what is this process called? | back 120 break lipid droplets apart; emulsification |
front 121 where is the pancreas | back 121 posterior to the stomach |
front 122 what are the three parts of the pancreas? | back 122 head body and tail |
front 123 what does the pancreatic duct meet and where? what does it do? | back 123 common bile duct at duodenal papilla and drains pancreatic juice into duodenum |
front 124 what occurs in 3% to 10% of people | back 124 accessory pancreatic duct |
front 125 what are pancreatic acini? what do they secrete? | back 125 organizational units made from pancreatic aciner cells; pancreatic enzymes |
front 126 what can peridontal disease cause? | back 126 gingivitis, tooth decay, and tooth loss |
front 127 what is mumps? where is it usually? | back 127 infection of salivary glands; parotid salivary gland |
front 128 what other organs can mumps affect? | back 128 gonads and meninges |
front 129 what is esophagitis usually caused by? | back 129 escaping stomach acids (GERD) |
front 130 what can cause hepatitis? | back 130 drugs, alcohol, or infection |
front 131 what is cirrhosis? | back 131 replacement of hepatocytes with scar tissue |
front 132 what do the hepatitis viruses do? | back 132 destroy the liver cells |
front 133 what causes the yellowness if skin and eyes with juandice? | back 133 accumulation of bilirubin |
front 134 what are gallstones? | back 134 crystals of insoluble minerals and salts forming when bile becomes too concentrated. |
front 135 what causes cholecystitis? | back 135 when gallstones block cystic duct |
front 136 what can cause pancreatitis? where is it normally found? | back 136 duct blockage, viral infection, or toxic drugs; dogs |
front 137 what are two types of peptic ulcers? | back 137 gastric and duodenal |
front 138 what are over 80% of ulcers caused by? what are treatments for ulcers? | back 138 infection of helicobactor pylori bacterium; acid reducers or antibiotics for h. pylori if present. |
front 139 what is what cause of enteritis and what does this disease cause? | back 139 infection by hiardia lamblia; diarrhea |
front 140 what is dysentery and what does it cause? | back 140 inflammation of small and large intestine and causes bloody diarrhea |
front 141 what gastritis? | back 141 inflammation of stomach lining |
front 142 what is gastroenteritis? what causes it and where is it ususally found? | back 142 inflammation of stomach lining and intestine; pathogenic infection and found often in areas with poor sanitation and low water quality |
front 143 what causes the diarrhea or constipation associated with colitis? | back 143 d- too much fluid or absorption capabilities compromised
|
front 144 what people are more susceptible to colerectal cancer? what does this disease begin as? | back 144 people over 50 with diets that are high in animal fat and low in fiber; small localized tumors. (polyps) |