What is the purpose of the Urinary system?
To filter the blood by removing _________ and __________________.
a. minerals and toxic waste
b. metabolic wastes and urea
c. toxins and metabolic wastes
c. toxins and metabolic wastes
Kidneys help maintain internal environment by :
Regulating total ________ volume and total concentration of ____________.
a. blood and electrolytes
b. electrolytes minerals
c. water and solutes
c. water and solutes
Kidneys help maintain internal environment by :
Regulating concentration of _________ in _________________
a. ions, intracellular fluids
b. ions in extra-cellular fluids
c. minerals body electrolytes
b. ions in extra-cellular fluids
Kidneys help maintain internal environment by
a. by ensuring homeostatic acid-base balance, pH of body
b. maintaining hydrostatic pressure in the filtered blood
c. maintaining balance of renin-angiotensin aldosterone mechanism
a. by ensuring homeostatic acid-base balance, pH of body
Kidneys help maintain internal environment by
a. providing sodium transport from cells to kidney filtration nephrons
b. providing a transport maximum for proteins out of the cell membrane
c.excreting metabolic wastes, foreign substances and toxins
c.excreting metabolic wastes, foreign substances and toxins
Kidneys help maintain internal environment by:
a.) regulates the rate of filtrate formation and systemic blood pressure
b. producing renin and erythropoietin for regulating bp and Red blood cell production
c.Its macula densa cells produce aldosterone.
b. producing renin and erythropoietin for regulating bp and Red blood cell production
Kidney help maintain internal environment by:
a. Converting Vit D to its active form
b. synthesizing ADH and aldosterone in the nephrons
c. maintaining constant GFR rate
a. Converting Vit D to its active form
Kidneys help to maintain internal environment by?
a. help regulate blood pressure and the rate of blood filtration GFR
b. monitor the NaCl content of the filtrate entering the distal convoluted tubule.
c. performing gluconeogenesis during prolonged fasting
c. performing gluconeogenesis during prolonged fasting
Kidneys filter almost _______ liters of blood per day
a. 150
b. 200
c. 350
b. 200 liters per day or 48-50 gallons or my total blood volume 36 times per day
What are the ureters:
a. a muscular sac that lies posterior to the pubic symphisis
b. a muscular tube that conveys urine from the bladder to the body exterior
c. slender tubes running from each kidney to the bladder
c. slender tubes running from each kidney to the bladder
What is the urethra:
a. a muscular tube that conveys urine from the bladder to the body exterior
b. a tube that connects the glomerular capsule to the nephron loop
c.c. slender tubes running from each kidney to the bladder
a. a muscular tube that conveys urine from the bladder to the body exterior
What is a nephron?
a. a funnel shaped tube continous with the ureter leaving the hilum
b. a variable network of autonomic nerve fibers found in the cortex of the kidneys
c. the structural and functional units of the kidneys, blood processing units that form urine
c. the structural and functional units of the kidneys, blood processing units that form urine
They are mostly located in the cortex, 85% located here
Each nephron consists of _________ and a ________.
a. medulla and cortex
b. proximal convoluted tube and distal convoluted tube
c. a renal corpuscle and a renal tubule
c. a renal corpuscle and a renal tubule
all the renal corpuscles are located in the renal cortex.
the tubules begin in the cortex and then pass into the medulla
What does each renal corpuscle consists of?
a. a nephron loop and proximal convoluted tubule cells
b. a collecting duct tube and a distal convoluted tubule
c. a tuft of capillaries called glomerulus and it is surrounded by a glomerular capsule
c. a tuft of capillaries called glomerulus and it is surrounded by a glomerular capsule
glomerular capsule is continous with its renal tubule.
What type of endothelium makes up the glomerular capillaries and why is this important?
a. stratified columnar cells with villi which allow large amounts of solute rich fluids into the glomerular capsule to be processed in renal tubules to form urine
b. fenestrated-many pores, allow large amounts of solute rich fluids to pass into glomerular capsule to be processed in renal tubules to form urine.
c. simple squamous epithelium which contributes to the capsule structure, supports capillaries but plays no part in forming filtrate.
b. fenestrated-many pores, allow large amounts of solute rich fluids to pass into glomerular capsule to be processed in renal tubules to form urine
The glomerular capsule has an external ______ layer and a ______ layer that clings to the glomerular capillaries.
a. endothelial , parietal
b. brush border, visceral
c. parietal, visceral
c. parietal, visceral
The visceral layer which clings to the glomerular capillaries consists of highly modified branching epithelial cells called
a. pseudopods which terminate in foot processes
b. pedal villi which terminate in foot processes
c. podocytes which terminate in foot processes
c. podocytes which terminate in foot processes
How does the glomerulus differ from all other capillary beds in the body?
a. It is both fed and drained by arterioles, fed by the afferent arteriole and drained by the efferent arteriole.
b.It is both fed and drained by venules, fed by the afferent venule and drained by the efferent venule.
a. It is both fed and drained by arterioles, fed by the afferent arteriole and drained by the efferent arteriole.
NORMALLY A CAPILLARY SENDS BLOOD TO A VENULE
Glomerular capillaries have a filtration member over _______ more permeable than ordinary capillaries. Also have a filtration pressure __________.
a. 200 times, 1.5x higher
b. 500 times, 2x higher
c. 1000 times, 3x
c. 1000 times, 3x
Blood coming into the nephrons is ___________ blood , it comes out ________.
a. unloaded, filtered
b. loaded, filtered
c. saturated, filtered
b. loaded, filtered
What are the three processes of urine formation?
a. Renal autoregulation, tubuloglomerular mechanism and filtration
b. glomerular filtration, tubular reabsorption, tubular secretion
c. glomerular filtration, renal autoregulation, passive paracellular division
b. glomerular filtration, tubular reabsorption, tubular secretion
What happens during glomerular filtration?
a.Diameter of glomerular capillaries increases to maintain normal glomerular filtration rate
b. movement of substances from the glomerulus into the renal tubule due to hydrostatic pressure-electrolytes, toxins, metabolic wastes.
c. Water and solubles are reabsorbed, the loop first concentrates the filtrate, then dilutes it.
b. movement of substances from the glomerulus into the renal tubule due to hydrostatic pressure-electrolytes, toxins, metabolic wastes.
Proteins and Red blood cells are not filtered
What happens during tubular reabsorption?
a. reabsorption of minerals from the the interstitial fluid to the tubules
b. movement of substances from the capillaries to the tubules
c. movement of substances from the filtrate to the capillaries- Desirables
c. movement of substances from the filtrate to the capillaries- Desirables
tubular reabsorption, quickly reclaims most of the tubule contents and returns them to the blood.
Sodium ions are the single most abundant cation in the filtrate.
What happens during tubular secretion?
a. it is the movement of solutes following solvents along their concentration gradients into the peritubular capillaries
b. Transmembrane proteins, aquaporins, found in the tubules act as water channels across plasma membrane of the tubules
c. movement of selected substances from the capillaries to the tubule, undesirable substances
c. movement of selected substances from the capillaries to the tubule, undesirable substances
TUBULAR SECRETION IS IMPORTANT FOR:
DISPOSING OF SUBSTANCES IE DRUGS AND METABOLITES THAT ARE TIGHTLY BOUND TO PLASMA PROTEINS
ELIMINATING UNDESIRABLE SUBSTANCES OR END PRODUCTS THAT HAVE BEEN REABSORBED BY PASSIVE PROCESSES, IE UREA AND URIC ACID
RIDDING THE BODY OF EXCESS POTASSIUM K+
CONTROLLING BLOOD pH
Path of urine collection in the kidney?
Several collecting ducts drain into a minor calyx
several minor calyces drain into a major calyx
several nephrons drain into a common collecting duct
renal pelvis drains into ureter
all major calyces drain into the renal pelvis
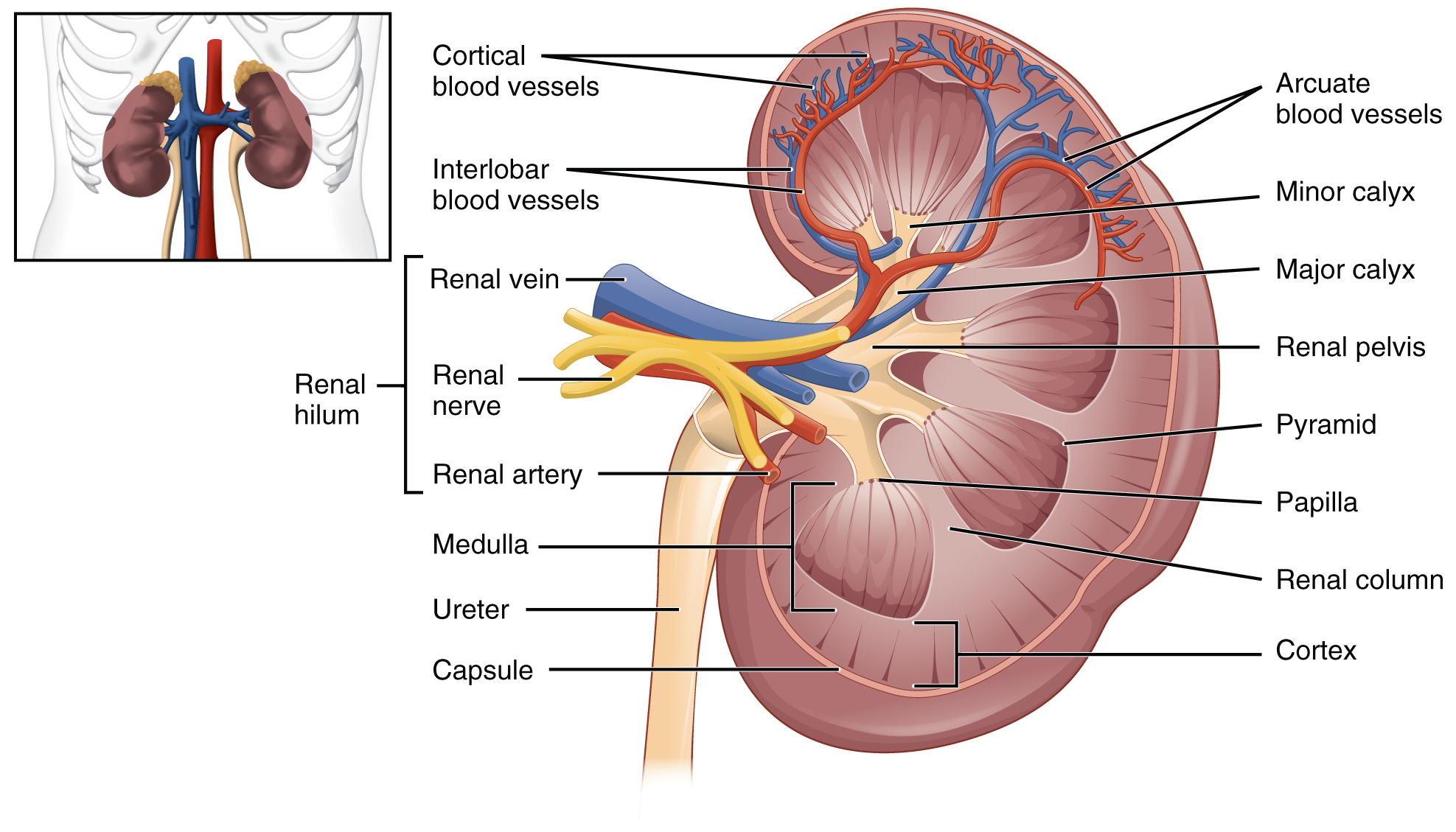
1. several nephrons drain into a common collecting duct
2. Several collecting ducts drain into a minor calyx
3.several minor calyces drain into a major calyx
4. all major calyces drain into the renal pelvis
5. renal pelvis drains into ureter
What is the glomerular filtration rate?
a.Amount of substance excreted in urine per minute:
b. Glomerular Hydrostatic pressure minus Capsular hydrostatic pressure
c. the rate at which blood is filtered
c. the rate at which blood is filtered
APPROX 125 ml/min OR 180 LITERS, (48 GALLONS/DAY)
The higher the _____________, the greater the _______________.
a. renal clearance, GFR
b. net filtration pressure, GFR
b. net filtration pressure, GFR glomerular filtration rate
Changes in blood pressure can significantly affect the filtration pressure, and thus filtration.
A ______ drop in arterial blood pressure can result in total loss of filtration _____.
a. 5%, dysuria
b. 10% , polyuria
c. 15%, anuria
c. 15%, anuria
What happens when bp gets too low?
a. bradycardia, hypoxia occurs
b. tachycardia, acidosis occurs
c. kidney failure , toxemia occurs
c. kidney failure , toxemia occurs
What is renal clearance?
a. renal blood vessels are dilated and renal autoregulation prevails
b. the kidneys maintaining a constant GFR despite fluctuations in systemic arterial bp
c. the kidney's ability to remove a substance from the blood in a given amount of time( ml/min)
c. the kidney's ability to remove a substance from the blood in a given amount of time( ml/min)
Substances completely reabsorbed, such as glucose, have a clearance factor of?
a. 1
b.2
c. zero
c. zero
What are clearance tests used for?
a. to evaluate nephron capacity and GFR rate
b. to evaluate filtering rate of glomerulus and disease
c. to evaluate kidney function, detect presence of substances in urine
c. to evaluate kidney function, detect presence of substances in urine
Tubular reabsorption "reclaiming what the body needs to keep" is the process of selectively moving substances from the filtrate back into the blood.Keeps glugose and amino acids.
It takes place in the renal tubules and collecting ducts.
What percent of the filtrate becomes urine and leaves the body?
a. 10%
b. 1%
c. 15%
b. 1%
99% is reabsorbed
What would happen if reabsorption stopped?
a. body would lose most of its fluids and renal activity would slow down
b. the entire vascular system would be drained in 1 hour
c. the kidneys and tubules would become engorged and stop functioning
b. the entire vascular system would be drained in 1 hour
Tubular reabsorption is specific process, substances are reabsorbed at specific points along the tubule in specific amounts. It depends upon the body's need for the substance at any given time.
a. true
b. false
a. true
Most nutrients such as ______, _______, _________ and many _______ are extensively reabsorbed.
a. minerals, ions, vitamins, substances
b. nucleic acids, lipids, hormones, lymph
c. amino acids, glucose, electrolytes and drugs
c. amino acids, glucose, electrolytes and drugs
In tubular reabsorption, are waste products reabsorbed? No
what are some waste products?
a. potassium, urea, pancreatic acid
b. electrolytes, ions, creatinine
c. urea, creatinine, uric acid
c. urea, creatinine, uric acid
What is involved in tubular secretion step 3 of urine formation?
a.H+ is secreted and makes the blood more alkaline and urine more acidic
b. The transporters are saturated, the excess is secreted in urine
c. process of selectively moving substances from the blood to the filtrate, from the peritubular capillaries to the filtrate
c. process of selectively moving substances from the blood to the filtrate, from the peritubular capillaries to the filtrate
Tubular secretion is important for:
TUBULAR SECRETION IS IMPORTANT FOR:
DISPOSING OF SUBSTANCES IE DRUGS AND METABOLITES THAT ARE TIGHTLY BOUND TO PLASMA PROTEINS, penicillin
ELIMINATING UNDESIRABLE SUBSTANCES OR END PRODUCTS THAT HAVE BEEN REABSORBED BY PASSIVE PROCESSES, IE UREA AND URIC ACID, creatinine, ammonia
RIDDING THE BODY OF EXCESS POTASSIUM K+
CONTROLLING BLOOD pH
Tubular secretion disposes of waste and /or toxic substances. It is the only way to dispose of?
a. excess sodium
b. excess potassium
c. excess urea and ammonia
b. excess potassium
H+ is secreted during tubular secretion, it makes the blood more ________ and the urine more _______
a. basic , alkaline
b. alkaline, acidic
b. alkaline, acidic
What type of cells is the Juxtaglomerular Apparatus made of?
a.Proximal tubule cell, endothelial cells, granular cells
b. granular cells, basilar cells, mechanoreceptor cells
c. granular cells, macula densa cells, extraglomerular mesangial cells
c. granular cells, macula densa cells, extraglomerular mesangial cells
what do the Juxtaglomerular cells help regulate?
a. renal blood pressure and filtrate volume
b. systemic blood pressure and rate of filtrate formation
c. systemic blood pressure and net filtration pressure
b. systemic blood pressure and rate of filtrate formation
What are granular cells found at the juxtaglomerular apparatus made of?
a. simple cuboidal with many microvilli and many mitochondria, contain renin
b. simple squamous epithelium in the afferent arterioles of juxtamedullary nephrons
c. modified smooth muscle cells in the afferent arterioles of juxtamedullary nephrons, have secretory granules, contain renin
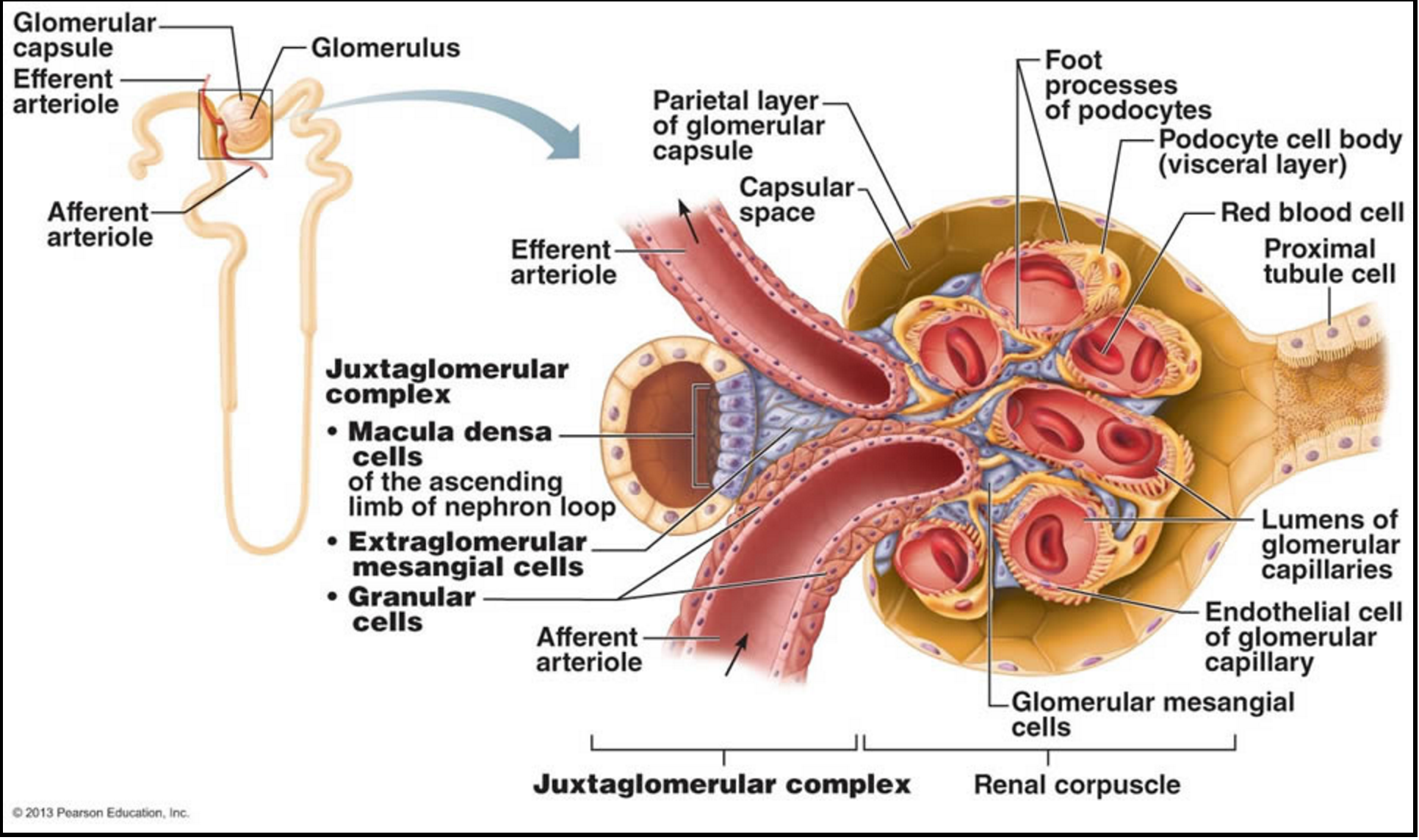
c. modified smooth muscle cells in the afferent arterioles of juxtamedullary nephrons, have secretory granules, contain renin
Where are macula dense cells found and what do they monitor?
a. located in the proximal convoluted tubule, adjacent to the Juxtaglomerular Apparatus, have baroceptors that monitor pressure in the afferent arterioles
b. located in the distal renal tubule, adjacent to the Juxtaglomerular Apparatus, have chemoreceptors that monitor NaCl content of filtrate in afferent arteriole.
c. located in the vasa recta, adjacent to cortex-medulla junction, monitor pressure in the efferent arterioles
b. located in the distal renal tubule, adjacent to the Juxtaglomerular Apparatus, have chemoreceptors that monitor NaCl content of filtrate in afferent arteriole.
What are the extraglomerular mesangial cells?
a. mechanoreceptor cells that sense the blood pressure in the afferent arteriole
b. simple cuboidal with many microvilli and many mitochondria, contain renin
c.pass signals between macula densa cells and granular cells
c.pass signals between macula densa cells and granular cells
Regarding renal control of blood pressure, what do granular cells JGA monitor?
a. the hydrostatic pressure in glomerular capillaries, glomerular blood pressure
b. the degree of stretch(pressure) on the walls of the afferent arteriole-one bringing blood in
c. the hydrostatic pressure in the glomerular capsule space
b. the degree of stretch(pressure) on the walls of the afferent arteriole-one bringing blood in
How do granular cells respond to low blood pressure?
a. by releasing Angiotensin II
b. by releasing renin into the blood
c. by releasing aldosterone into the blood
b. by releasing renin into the blood
RENIN BEGINS A CASCADE OF EVENTS THAT RAISE BLOOD PRESSURE
Renin converts ______________ to _______________.
a. ADH to aldosterone
b. creatinine to creatine
c. angiotensinogen, angiotensin I
c. angiotensinogen, angiotensin I
Angiontensinogen is an inactive liver protein
How is Angiotensin I transfomed to Angiotensin II?
a. accomplished by ADH as it passes through the kidneys
b. accomplished by Aldosterone as it passess through the kidneys
c. accomplished by angiotensin converting enxyme (ACE) as it passes through the lungs
c. accomplished by angiotensin converting enxyme (ACE) as it passes through the lungs
Angiotensin II acts directly on blood vessels, causing their constriction and thereby raising blood pressure.
Drugs that inhibit ACE, and thus block the conversion of angiotensin I to angiotensin II, are used to lower blood pressure in patients with hypertension
What happens as Angiotensin II causes vasoconstriction of systemic arterioles?
a.blood volume and pressure decreases, glomerular filtration rate increases, adrenal gland secretes ADH
b. blood pressure increases, Net filtration pressure increases-ensures that some excretion will continue despite low BP, adrenal cortex releases aldosterone
c. blood pressure decreases, Net filtration pressure decreases, ensures some excretion will continue despite low BP, adrenal cortex releases renin
b. blood pressure increases, Net filtration pressure increases-ensures that some excretion will continue despite low BP, adrenal cortex releases aldosterone.
Angiotensin II is a potent vasoconstrictor that stimulates aldosterone secretion
What does aldosterone released by the adrenal cortex do?
a. Acts to conserve potassium, increases potassium reabsorption by the kidneys.
b. Acts to conserve sodium, increases sodium reabsorption by the kidneys and conserves sodium in saliva, stomach, perspiration
c. inhibits Angiotensin effects and increases blood volume
b. Acts to conserve sodium, increases sodium reabsorption by the kidneys and conserves sodium in saliva, stomach, perspiration
WATER IS PASSIVELY REABSORBED WITH THE SODIUM Na+ TO INCREASE BLOOD VOLUME.
WATER FOLLOWS SODIUM Na+, if sodium is reabsorbed, water will also be reabsorbed
What does dehydration-lack of sufficient water in the body produce?
a. a low osmotic pressure in the blood due to decreased concentration of plasma proteins.
b. a high osmotic pressure in the blood due to increased concentration of plasma proteins
b. a high osmotic pressure in the blood due to increased concentration of plasma proteins
Osmoreceptors in the _______________ and the ______________ respond to _____________.
a. granular cells and the pons, decrease in bp
b. glomerular cells and the medulla , increase in bp
c. macula densa cells , hypothalamus, dehydration
c. macula densa cells , hypothalamus, dehydration
THE HYPOTHALAMUS CAUSES THE RELEASE OF ANTIDIURETIC HORMONE -ADH- FROM THE POSTERIOR PITUITARY
Blood volume and blood pressure are ______ related. If blood volume ________, pressure _________.
a. inversely, increases, decreases
b. equally , remains stable, remains stable
c. directly, increases, increases
c. directly, increases, increases
How do Antidiuretic hormones act?
a. increased perpiration, decreased permeability of the distal and collecting tubes
b. decreased perspiration, increased permeability of the distal and collecting tubules
b. decreased perspiration, increased permeability of the distal and collecting tubules
increased permeability of tubules allows more water to pass from filtrate into the blood- antidiuretic effect
increased water reabsorption dilutes the blood , expands blood volume and raises blood pressure
Blood pressure can also be increased directly by ADH.
a. usually occurs with severe electrolyte loss due to perspiration
b. usually occurs with severe blood loss due to hemorrhage
b. usually occurs with severe blood loss due to hemorrhage
What is the bladder and its function?
a. primarily skeletal muscle, stores urine temporarily, can hold about 1000 ml of urine
b. primarily made of collagen fibers, stores urine, can hold about 500 ml of urine
c. primarily smooth muscle, very stretchable, stores urine temporarily, can hold about 800 ml of urine
c. primarily smooth muscle, very stretchable, stores urine temporarily, can hold about 800 ml of urine
What follows when there is increased pressure in the bladder?
a. the opening of the ureters open
b. the openings of the ureters and urethra open
c. the openings of the ureters close.
c. the openings of the ureters close.
THERE ARE NO SPHINCTERS OR VALVES
PREVENTS BACKFLOW OF URINE TO THE KIDNEYS
The urethra has how many sphincters that keep urine from leaking from the bladder ?
a. one internal sphincter
b. an internal urethral sphincter and an external sphincter
b. an internal urethral sphincter and an external sphincter
What is an infection of the bladder called?
a. glomerulonephritis
b. pyelonephritis
c. cystitis
c. cystitis
Micturition Reflex-When about 200 ml of urine accumulate, what receptors send impulses to the sacral region of the spinal cord?
a. mechanoreceptors in the urinary bladder
b. baroreceptors in the bladder
c. stretch receptors in the urinary bladder
c. stretch receptors in the urinary bladder
What is the next event in micturition?
a. the external sphincter relaxes and the bladder reflexively contracts
b. contractions temporarily cease until enough urine is collected
c. smooth muscles begin rhythmic contractions which send impulses to the cerebral cortex which produce a desire to urinate.
c. smooth muscles begin rhythmic contractions which send impulses to the cerebral cortex which produce a desire to urinate.
The pons is the part of the brain that controls the micturition reflex
What happens when desire to urinate is postponed?
a. contractions continue to increase, until bladder is completely full
b. contractions temporarily cease until about 200 ml more urine collects
c. contractions build up until about 500 ml more urine collects.
b. contractions temporarily cease until about 200 ml more urine collects
when voiding occurs, the external sphincter relaxes and the bladder reflexively contracts.
What is the normal volume of urine excreted in 24 hour period?
1000-2000ml; 1-2 liters
THIS IS PRIMARILY DEPENDENT UPON INTAKE OF FLUIDS
Volume of Urine produced is affected by ADH when:
a. the pons recognizes concentrated blood, hyperosmolality
b. the hypothalamus recognized concentrated blood, hyperosmolality
b. the hypothalamus recognized concentrated blood, hyperosmolality
Urine volume is also affected by diuretics such as
a. caffeine and alcohol
b. aldosterone and alcohol
c. hormones and alcohol
a. caffeine and alcohol
What is the pH of urine?
a. slightly acidic, about 6.0-
b. slightly alkaline about 12.0
a. slightly acidic, about 6.0-